Description of Radial Endobronchial Ultrasound Miniature Probes (EBUS) in Pulmonary Medicine
Author: Prof. Felix JF Herth, MD, PhD, DSc, Thoraxklinik, University of Heidelberg, Germany
Source: DVD-ROM ‘Endoscopic Ultrasound – Diagnostics and Staging of Lung Cancer’, Olympus Europa SE & Co. KG, 2013
Improving Diagnostics of the Airways
Many pathologies, benign and malignant, of the airways involve the bronchial wall and the parabronchial structures. Radiological imaging has been proven to be unreliable in the diagnostics of these structures.
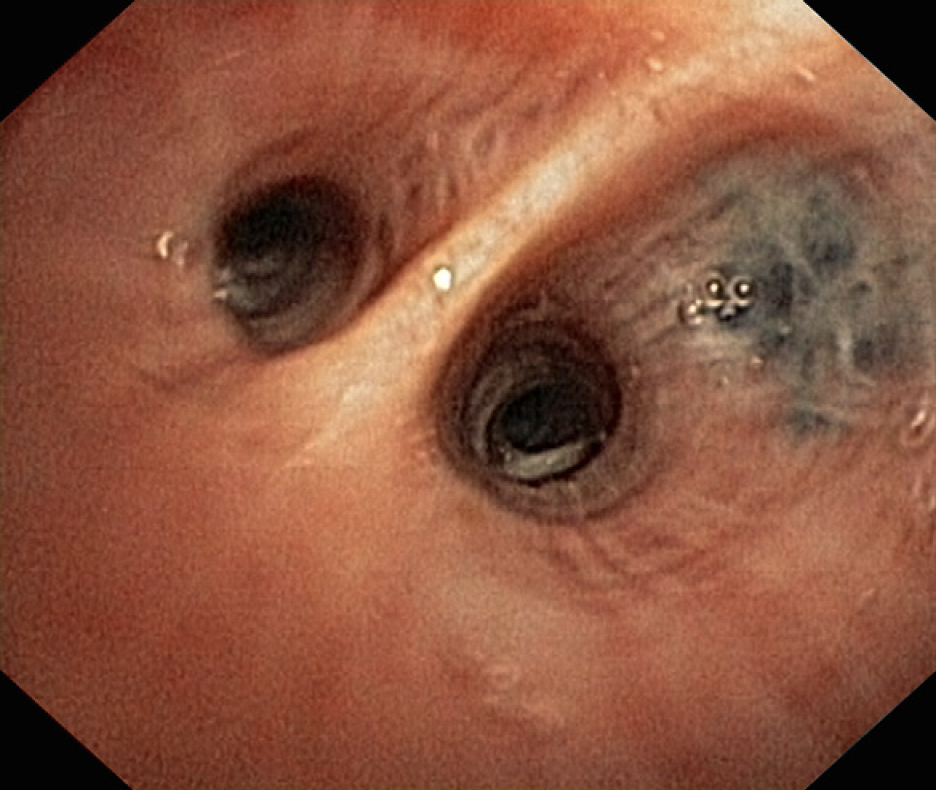
In routine bronchoscopy, the view of the endoscopist is limited to the lumen and the internal surface of the airways. Therefore, expanding the endoscopist’s view beyond the airways was an essential requirement to improve diagnostics.
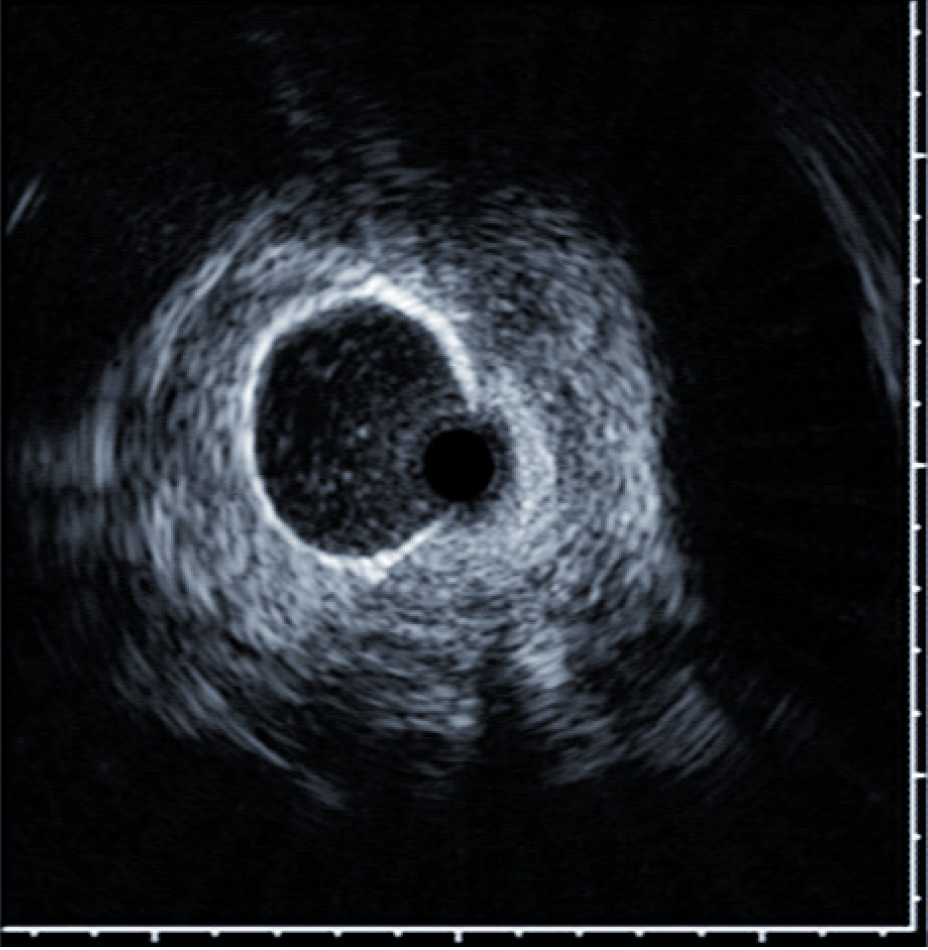
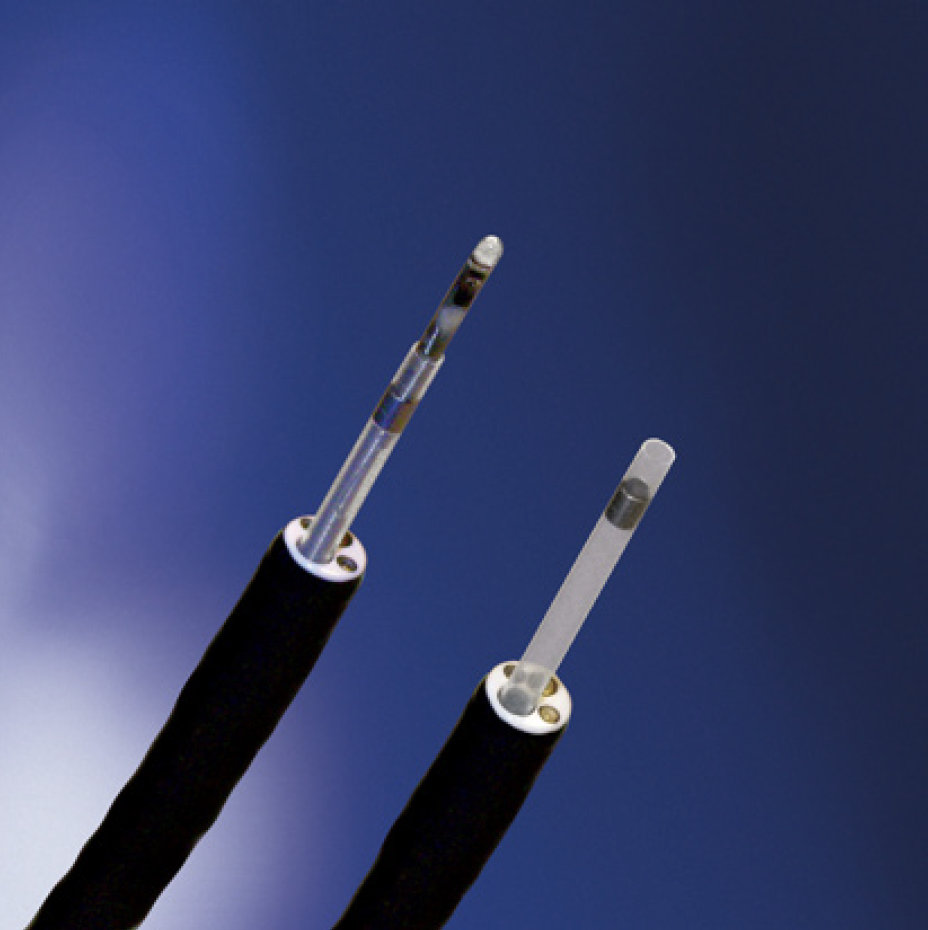
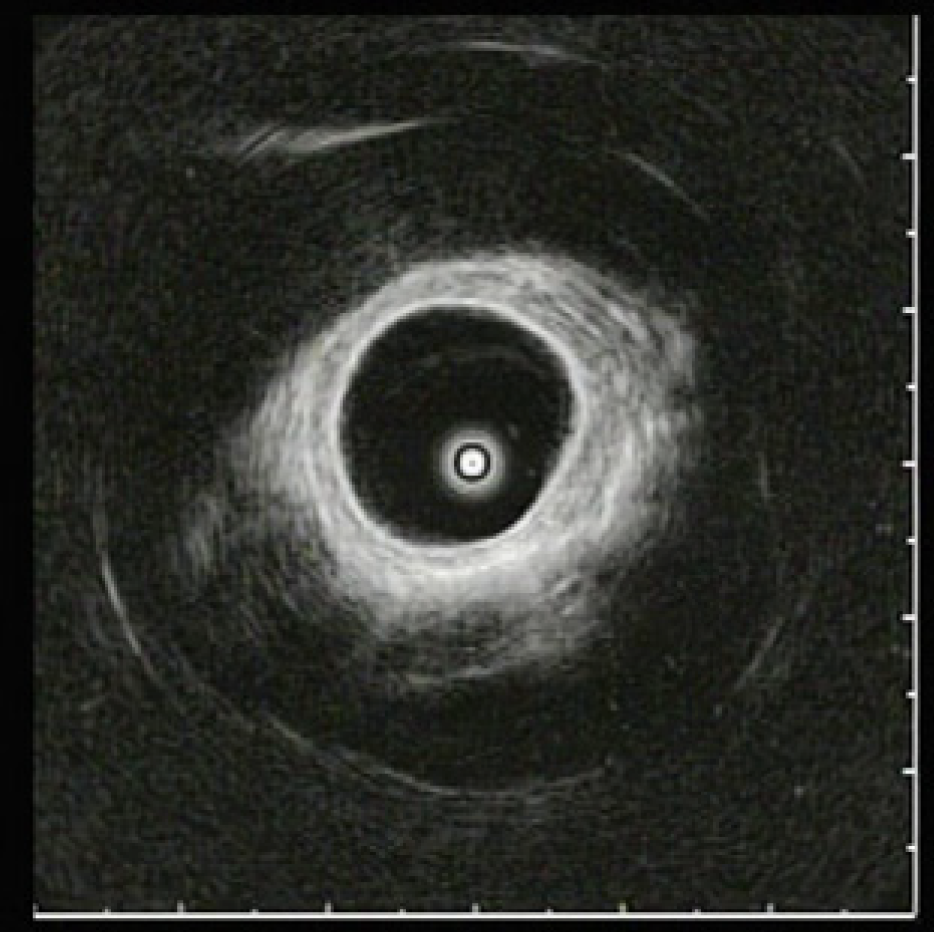
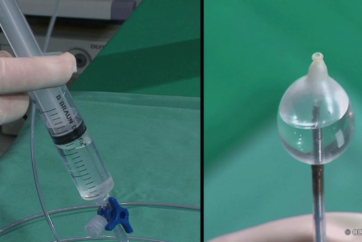
For application inside the airways, Olympus developed radial endobronchial ultrasound miniature probes (EBUS), catheters as well as catheters with a balloon at the tip that allow circular contact also in the larger lumen. Radial EBUS probes provide a complete 360° image of the parabronchial structures and under favourable conditions visualise structures up to a distance of 4 cm.
Peripheral Lesions (SPN)
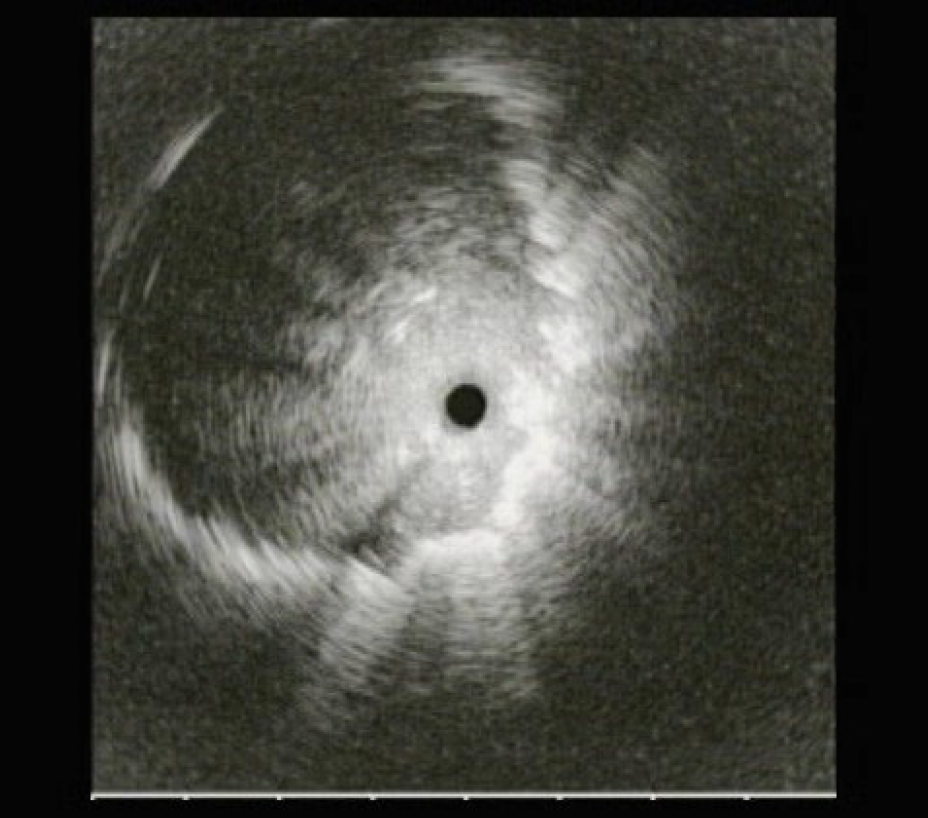
Solitary pulmonary nodules are an increasing diagnostic problem. Multiple approaches may be undertaken to establish a tissue diagnosis, including sputum cytology, percutaneous image-guided aspiration/biopsy, and bronchoscopic sampling. To obtain tissue samples for the histological evaluation of peripheral lesions, bronchoscopy under fluoroscopy is the standard procedure. This demands expensive x-ray equipment in the bronchoscopy suite or coordination with the radiology department and causes exposure to radiation for patient and staff. An important factor affecting the yield is that lesions situated beyond the airway lumen are not visible to the bonchoscopist, resulting in ‘blind’ biopsies. Fluoroscopy offers some assistance for localizing such lesions, especially in lesions larger than 3 cm. The two-dimensional projection views produced by fluoroscopy often do not show smaller lesions. In such lesions, mostly peripheral pulmonary lesions not visible endobronchially, diagnostic yield of routine bronchoscopy may therefore be less than 20%. The highest diagnostic yield for bronchoscopic evaluation of small SPNs appears to be associated with the use of radial ultrasound miniature probes (EBUS) in the diagnostic procedure. EBUS miniature probes employ a flexible catheter, housing a mechanically rotated ultrasound transducer which produces a 360° radial ultrasound image. The technique to use a miniature probe to guide TBLB was first described by Herth (Herth et al, Endobronchial Ultrasound-Guided Transbronchial Lung Biopsy in Solitary Pulmonary Nodules and Peripheral Lesions, Eur Respir J., 2002, Oct; 20(4), pp 972- 974) passing the probe into the bronchial subsegments until the characteristic ultrasound signal of a solid lesion is displayed. Numerous groups have published their experience with EBUS-guided evaluation of SPNs since.
A recent procedural improvement was achieved with the introduction of a guide sheath as an accessory to the EBUS probe. The sheath acts like a prolonged working channel of the bronchoscope and allows the removal of the probe after visualization of the solid lesion. With the distal end of the guide sheath still at the target site, sampling devices can then be brought forward. Specimens from four to six biopsies shall then be obtained through the guide sheath using regular biopsy forceps. Unfortunately the EBUS probes are not steerable. Therefore, navigation support (based on a virtual bronchoscopy calculated on CT data) is helpful to guide a thin bronchoscope close to the lesion. As the navigation systems lack the function to directly visualize the lesion, EBUS miniature probes should be used to confirm the location of the lesion before biopsy. Here, combining EBUS and navigation bronchoscopy improves the diagnostic yield of flexible bronchoscopy in peripheral lung lesions without compromising safety. This has been demonstrated for electromagnetic navigation bronchoscopy (ENB) by Eberhardt (Eberhardt et al., Multimodality Bronchoscopic Diagnosis of Peripheral Lung Lesions, Am J Respir Crit Care Med, 2007, Vol 176. pp 36-41) proving highest diagnostic result when combining ENB and EBUS. Recently it was also demonstrated by Asano and colleagues that virtual bronchoscopy combined with EBUS increases diagnostic yield (Asano et al., Virtual Bronchoscopic Navigation Combined with Endobronchial Ultrasound to Diagnose Small Peripheral Pulmonary Lesions, Thorax, published online July 11, 2011, doi: 10.1136/thx.2010.145490).
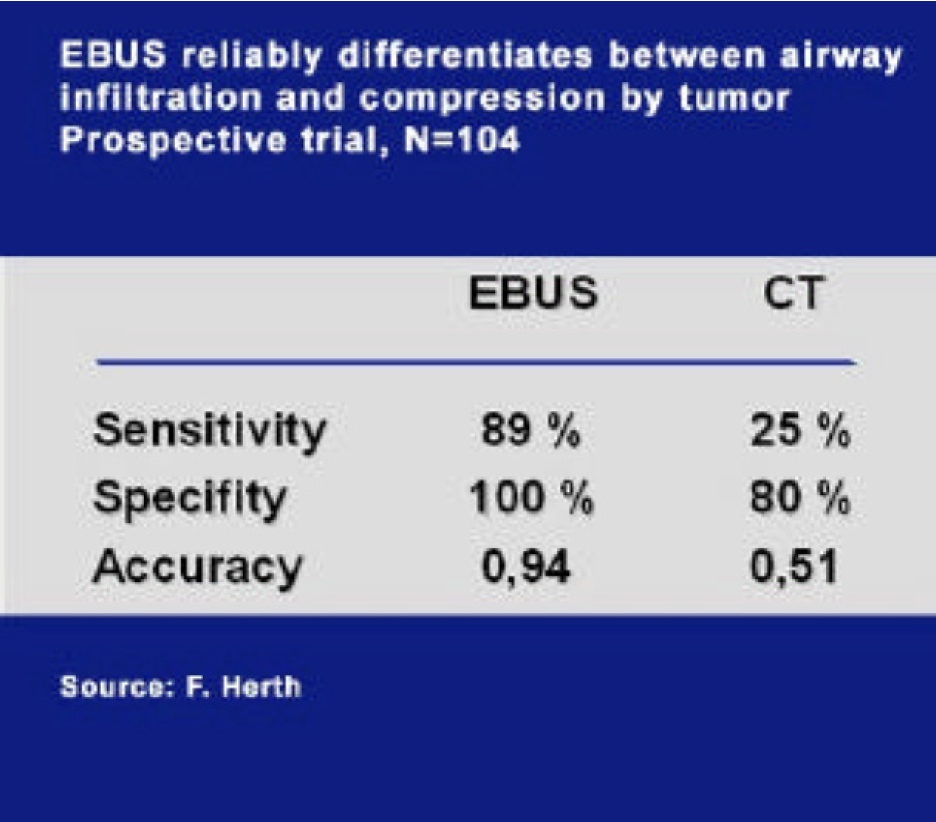
Invasion vs. Compression
In pre-operative staging, EBUS allows detailed analysis of intraluminal, submucosal and intramural tumour spread which can be essential for decision on resection margins. EBUS proved to be useful in the diagnostics of mediastinal tumour involvement like the large vessels and the oesophageal wall – which is frequently impossible with conventional radiology. In a prospective study, we could show that differentiation of external tumour invasion from compression of the tracheobronchial wall by EBUS is highly reliable in contrast to CT imaging (Herth et al., Endobronchial Ultrasound Reliably Differentiates Between Airway Infiltration and Compression by Tumor, Chest, 2003, 123, pp 458–462), thus many patients considered to be nonresectable by the radiologist due to supposed T4 tumours could be operated in a curative approach after EBUS.
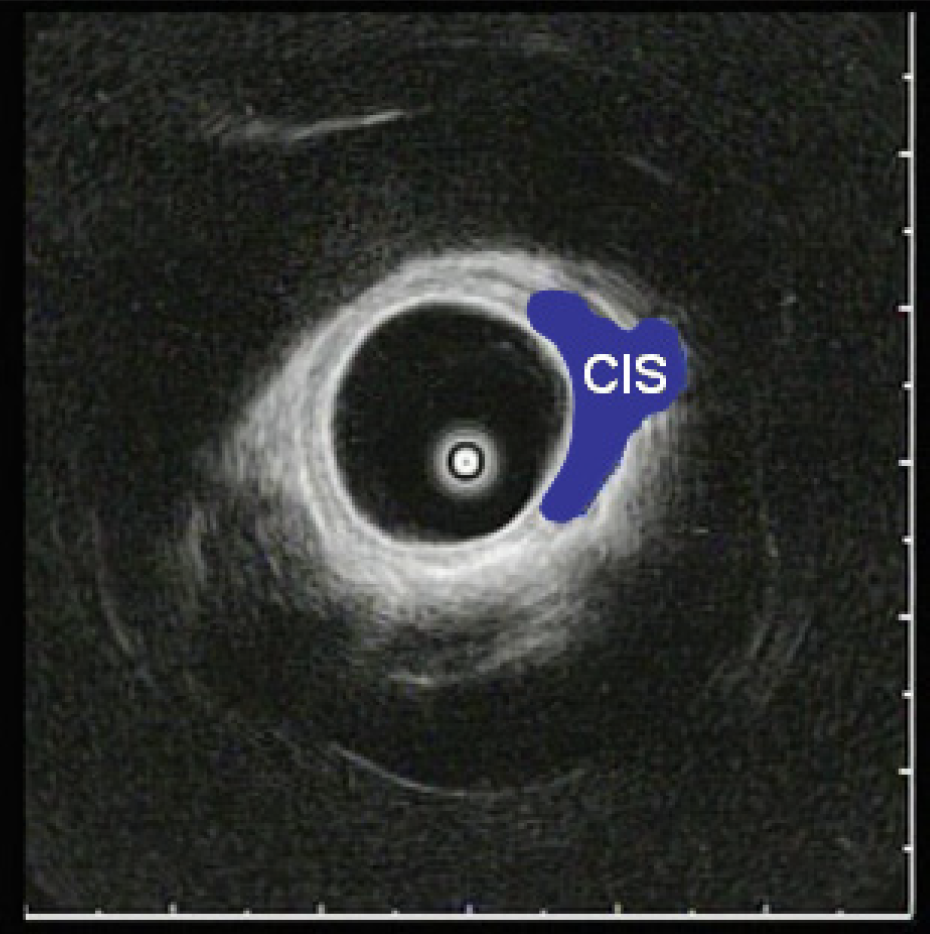
Early Cancer / CIS
In small radiologically invisible tumours like Carcinoma in Situ (CIS) the decision for local endoscopic therapeutic intervention is dependent on the tumour’s intraluminal and intramural extent within the multilayer structures of the bronchial wall and the adjacent structures.
EBUS is a very reliable tool in analysing the extent of these small lesions. Especially for decisions in potentially curative endobronchial therapy like photodynamic therapy or endoluminal high dose radiation, diagnosis of limitation of the lesion to the bronchial wall or to the close vicinity is essential. Here, EBUS is superior to all other imaging procedures due to the detailed analysis of the layers of the bronchial wall.
Conclusion
EBUS miniature probes have proven to be extremely useful. In many instances EBUS was superior for T-staging of lung cancer and for the diagnostics of other pathologies. EBUS is a valuable tool, especially for on-the-spot decision making during diagnostic and interventional procedures. With regards to the technique in clinical application and diagnostic results, radial endobronchial ultrasound is a routine procedure.