Esophageal ESD

Dr. Hiroyuki Ono, Division of Endoscopy, Shizuoka Cancer Center
Dr. Hiroyuki Ono contributed to the development of ITknife, ITknife2 and worked to advance the ITknife range to ITknife nano*, a device that is particularly suitable for esophageal and colorectal ESD. Here, Dr. Ono talks about esophageal ESD using ITknife nano. *Single Use Electrosurgical Knife KD-612
ITknife nano, a suitable knife for esophageal and colorectal application
Concept of ITknife nano
The new ITknife was developed to support a more secure and efficient ESD in the esophagus and colon. Since the development of ITknife2 was mainly for application in the stomach, the insulated tip was too large to be used in the esophagus where the submucosal layer is thin, making it difficult for the knife to slide under the submucosal layer. It was also found that the sparks from the electrode could easily reach the muscle layer causing problems such as exposure of the muscle layer or perforation.
To solve these problems, we invested considerable effort in determining the appropriate size of the insulated tip and electrode. We also pursued to make ITknife nano applicable for a constructed space and a thin submucosal layer such as the colon.
After various examinations, ITknife nano, a safe and efficient device for incision and dissection in esophageal and colorectal ESD, was developed. I am pleased with the outcome and have confidence that I have contributed to developing a good device. (Fig.1)

Fig.1:Easy to slide the knife under the submucosal layer
The smaller insulated tip can easily slide under the submucosal layer.Making incision and dissection safer
Among the ITknife users, some feel that ITknife2 cutting ability is too strong due to the electrode on the back of the insulated tip. I believe ITknife nano will be a good device for these users. In addition, ITknife nano can shorten the esophageal procedure time by 20 minutes on average compared to ITknife2 not only for those who are skilled at using it but also for those who have only experienced less than 30 cases of esophageal ESD using the device. This is because the feature of this knife is more suitable than ITknife2 for the use in the esophagus and users can manipulate the knife more easily. (Table) Since the spark of ITknife2 is stronger than the one of ITknife nano, we must be careful not to press ITknife2 forcefully against the organs which have thin submucosal layers. Pressing ITknife2 too hard can cause the current to reach the muscle layer. On the other hand, even if you apply the same force as ITknife2 for ITknife nano, the spark will remain in the submucosal layer due to its small disc-shaped electrode so it enables you to control the cutting easier. You can see from the table in page 3 that the risk of complications such as perforation and mediastinal emphysema can considerably be reduced when using ITknife nano in esophageal ESD. However, perforation and complications are a risk in any conditions even when ITknife nano is used. Thus, please avoid pressing ITknife nano on tissue excessively.
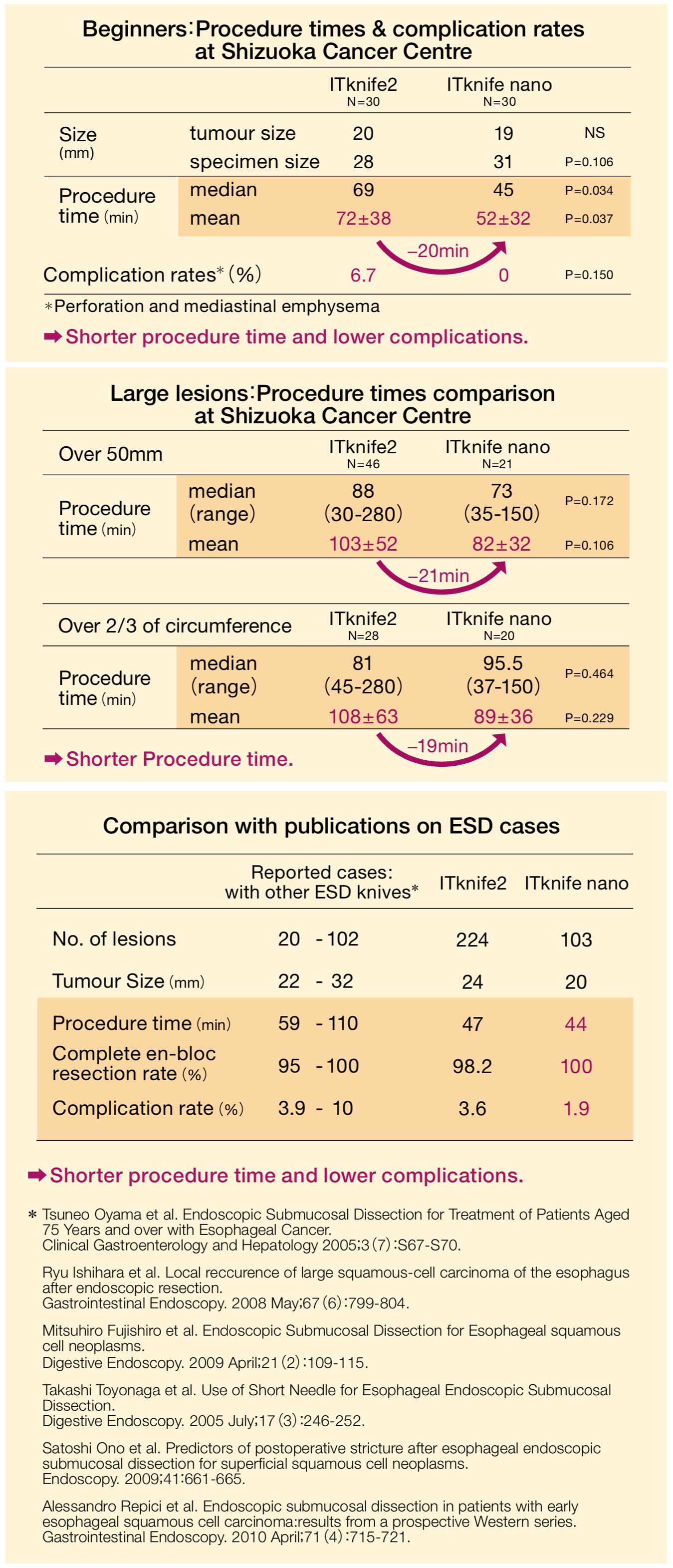
Table:Comparison of procedure time and complication rate of esophageal ESD
Tips for secure and efficient manipulation
Holding the knife upright for incision and dissection
There are some tips to perform secure ESD using ITknife nano in the esophagus. For circumferential incision, I hold the knife slightly upright so it does not damage the muscle layer. Next, it is essential to perform a certain amount of initial dissection in the distal side before starting dissection in the proximal side. Without this step, it will be difficult to identify the goal of the dissection. In addition, performing an adequate initial dissection on the distal side clarifies the edge of the submucosal layer and dissection becomes easier to perform. The submucosal dissection is performed by using the long blade and electrode which contributes to efficient dissection. Since the esophagus is a lumen, it is important to always be aware of the line and curve and manipulate the knife along it. At that time, always keep in mind to perform additional injection to lift up the submucosal layer and to keep the knife slightly upright. To avoid the knife cutting in too deep, it is essential to move the insulated tip together with the long blade. (Fig.2)
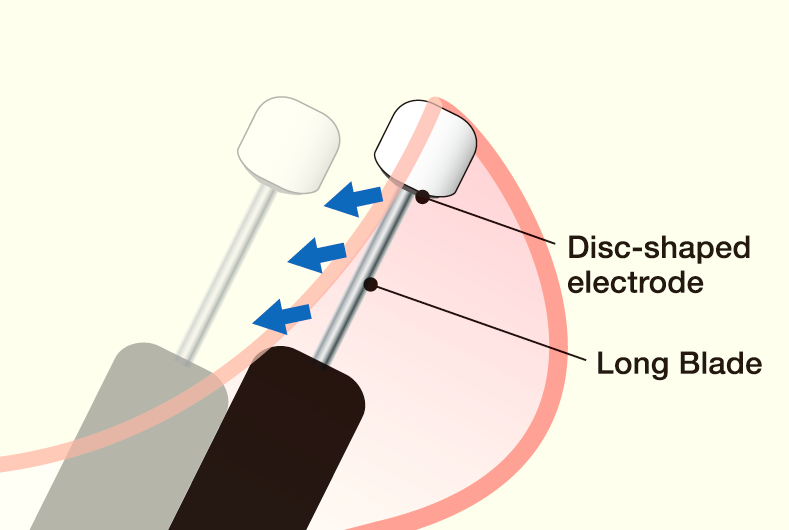
Fig.2:“Swing cut”: Sliding the knife fully under the mucosa
It is important to move the knife entirely including the insulated tip. This supports the knife to avoid cutting into the tissue deeply and helps a secure incision and dissection.Sufficient local injection and field of view
Caution is the key to ESD. In cases where the field of view is obscured by bleeding, the cutting line becomes difficult to identify. Performing dissection in this condition increases the risk of perforation. I myself have experienced perforation by pressing the ITknife toward the muscle layer in lesions where the cutting line was difficult to identify. It is essential to always maintain a clear field of view and lift up the submucosal layer. Additional injection is a solution to elevate the submucosal layer.
Recommendations for complicated esophageal cases
ESD in recurrent cases after EMR
ITknife nano is an extremely helpful instrument for fast and safe esophageal ESD. But there may be complicated situations where it may be advisable to consider also other treatment options. In my personal experience the most complicated cases are recurrent esophageal lesions with strong fibrosis, especially after repeated EMR & chemoradiation therapy. In such cases, the space of the submucosal layer becomes narrow and the border of the submucosal layer and muscle layer must be cut very cautiously. Making one wrong move may lead to perforation. Thus, in such cases with extremely difficult dissection, my recommendation is to consider carefully the full range of options for maximal patients safety:
Surgical treatment
Referal to a specialized facility with high experience in ESD (if the patient strongly requests endoscopic treatment).
Using (additionally) ESD knives of the "needle-type", such as DualKnife and or HookKnife.
Perform esophageal ESD under specialist supervision before mastering it
The main advantage of ESD compared to EMR is that the lesion can be resected en-bloc and more accurate pathological diagnosis is possible. For EMR, the rate of occurrence of remnant tissue rises for larger lesions. Even when the lesion is completely resected, accurate pathological diagnosis becomes difficult since the resected margin may be damaged with thermal denaturation and the depths of invasion cannot be diagnosed accurately. Consequently, the current way of thinking in Japan is to perform EMR if the lesion can be completely en-bloc resected by EMR and if not, perform ESD. Like other treatments, complications during ESD can lead to the patient’s death. Performing ESD for expanded lesions must be considered cautiously to prevent complications. In our facility, residents may only perform esophageal ESD after they are well trained and the supervising physicians agree they have enough skill to perform esophageal ESD. In my opinion, most people will be able to perform Gastric ESD without the guidance from the specialist after experiencing 50-60 cases. Esophageal ESD requires additional training after this, so mastering it needs at least a year or more. According to our data, in general, more than 90% of the physicians will reach the standard level of ESD after gaining experience in certain amount of cases.
Setting
| Electrosurgical unit | Treatment | Setting |
|---|---|---|
| VIO 300D | Mucosal Incision | EndoCutQ, Effect3, Cut Duration1, Cut Interval1 |
| Submucosal Dissection | SwiftCoag, Effect5, 45W |