NBI – REVIEW OF CLINICAL EVIDENCE 01
Diagnosis of narrow-band imaging in non-muscle-invasive bladder cancer: A systematic review and meta-analysis4
Kaiwen Li, Tianxin Lin, Xinxiang Fan, Yu Duan and Jian Huang
Objective
The objective was to evaluate the diagnostic accuracy of cystoscopy assisted by narrow-band imaging compared with white-light imaging for nonmuscleinvasive
bladder cancer.
Methods
An electronic database search of PubMed, Embase, the Cochrane Library, Ovid and Web of Science was carried out for all articles comparing narrow-band imaging with white-light imaging cystoscopy in the detection of non-muscle-invasive bladder cancer. The review process followed the guidelines of the Cochrane Collaboration.
Results
Seven studies with prospectively collected data including a total of 1040 patients were identified, and 611 patients with 1476 tumours were detected by biopsy.
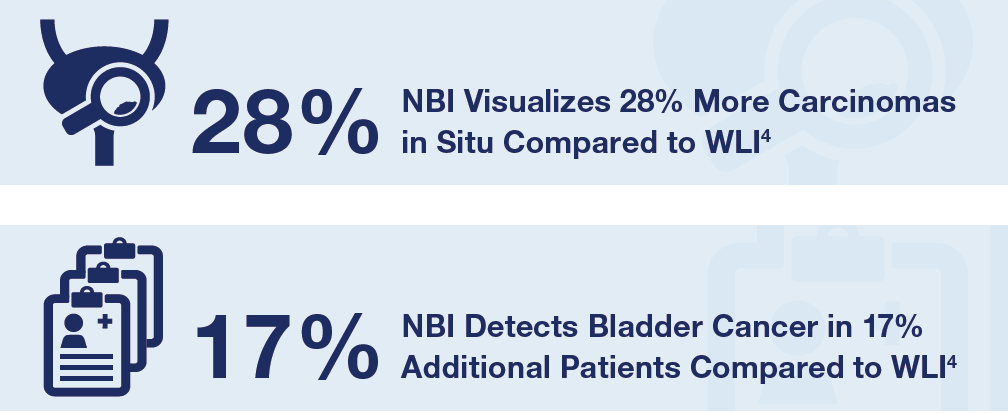
In the patient- and tumour-level analysis, an additional 17 % of patients (95 % confidence interval, 10–25 %)and an additional 24 % of tumours (95 % confidence
interval, 17–31 %) were detected by narrow-band imaging, respectively. In the patient- and tumour-level analysis, significantly higher detection rates using narrow-band imaging (rate difference 11 %; 95 % confidence interval 5–17 %; P < 0.001; and rate difference 19 %; 95 % confidence interval 12–26 %; P < 0.001, respectively) rather than white-light imaging were found. On the tumour level, an additional 28 % of carcinoma in situ was detected (95 % confidence interval 14–45 %) by narrow-band imaging, and a significantly higher detection rate (rate difference 11 %; 95 % confidence interval 1–21 %; P = 0.03) was found. The false-positive detection rate of tumour level did not differ significantly between the two techniques.
Conclusions
Cystoscopy assisted by narrow-band imaging detects more patients and tumors of non-muscle-invasive bladder cancer than white-light imaging, and it might be an additional or alternative diagnostic technique for nonmuscle- invasive bladder cancer.
Key Outcomes4
- Cystoscopy assisted by NBI detects more NMIBC patients and tumors than WLI.
- NBI is an alternative diagnostic technique for NMIBC.
- In the patient- and tumor-level analyses, an additional 17% of patients and an additional 24% of tumors were detected by NBI compared to WLI.
- On the tumor level, an additional 28% of carcinomas in situ were detected by NBI compared to WLI, and a significantly higher detection rate was found.
NBI – REVIEW OF CLINICAL EVIDENCE 02
Narrow band imaging-assisted transurethral resection reduces the recurrence risk of non-muscle invasive bladder cancer: A systematic review and meta-analysis3
Weiting Kang, Zilian Cui, Qianqian Chen, Dong Zhang, Haiyang Zhang and Xunbo Jin
Context
Compared with white light imaging (WLI) cystoscopy, narrow band imaging (NBI) cystoscopy could increase the visualization and detection of bladder cancer (BC) at the time of transurethral resection (TUR). NBI cystoscopy could increase the detection of BC, but it remains unclear whether narrow band imaging-assisted transurethral resection (NBI-TUR) could reduce the recurrence risk of non-muscle invasive bladder cancer (NMIBC). Several randomized clinical trials (RCTs) have recently tested the efficacy of NBI-TUR for NMIBC.
Objective
To perform a systematic review and meta-analysis of RCTs and evaluate the efficacy of NBI-TUR for NMIBC compared with white light imaging-assisted transurethral resection (WLI-TUR). The end point was recurrence risk.
Evidence Acquisition
A systematic review of PubMed, Medline, Ovid, Embase, Cochrane and Web of Science was performed in February 2016 and updated in July 2016.
Evidence Synthesis
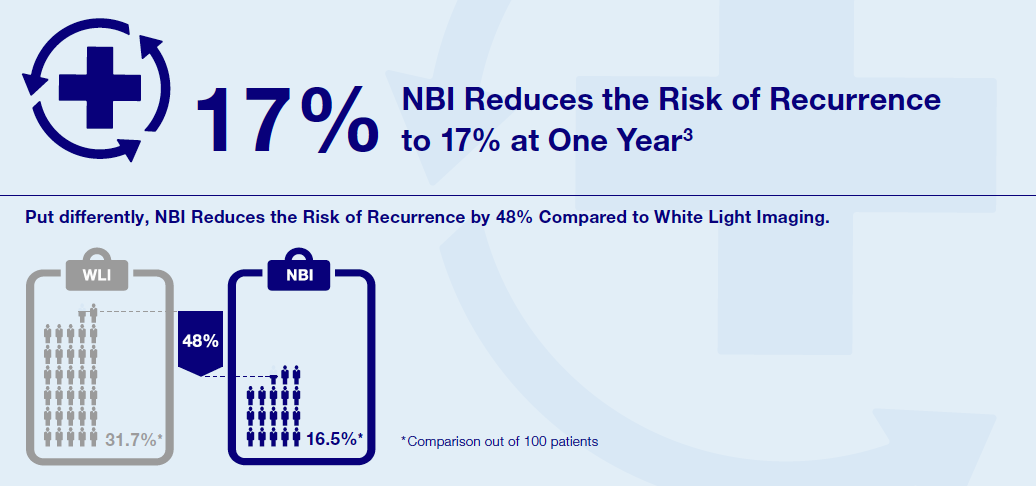
Overall, six (n = 1084) of 278 trials were included. Three trials performed narrow band imaging-assisted electro-transurethral resection (NBI-ETUR), and two trials performed narrow band imaging-associated bipolar plasma vaporization (NBI-BPV). The last trial performed narrow band imaging-associated holmium laser resection (NBI-HLR). Statistical analysis was performed using Review Manager software (RevMan v.5.3; The Nordic Cochrane Center, Copenhagen,Denmark). The recurrence risk was compared bycalculating risk ratios (RRs) with 95% confidenceinterval (CIs). Risk ratios with 95% CIs were calculatedto compare 3-mo, 1-yr, and 2-yr survival rates.NBI-TUR was associated with improvements in the3-mo recurrence risk (RR: 0.39; 95% CI, 0.26-0.60; p< 0.0001), 1-yr recurrence risk (RR: 0.52; 95% CI,0.40-0.67; p < 0.00001) and 2-yr recurrence risk (RR:0.60; 95% CI, 0.42-0.85; p = 0.004) compared withWLI-TUR.
Conclusions
Compared with WLI-TUR, NBI-TUR can reduce the recurrence risk of NMIBC. The results of this review will facilitate the appropriate application of NBI in NMIBC.
Key Outcomes3
- Compared with WLI cystoscopy, NBI cystoscopy increases the visualization and detection of bladdercancer.
- TUR-BT using NBI reduces the risk of NMIBC recurrence at three months, one year, and two yearssignificantly when compared with TUR-BT using WLI.
・At three months, NBI reduces the recurrence risk by 59.5% (NBI 6% vs WLI 14.8%).
・At one year, NBI reduces the recurrence risk by 48% (NBI 16.5% vs WLI 31.7%).
・At two years, NBI reduces the recurrence risk by 40% (NBI 17.7% vs WLI 29.5%).
NBI – REVIEW OF CLINICAL EVIDENCE 03
A network meta-analysis of therapeutic outcomes after new image technology-assisted transurethral resection for non-muscle invasive bladder cancer: 5-aminolaevulinic acid fluorescence vs hexylaminolevulinate fluorescence vs narrow band imaging8
Joo Yong Lee, Kang Su Cho, Dong Hyuk Kang, Hae Do Jung, Jong Kyou Kwon, Cheol Kyu Oh, Won Sik Ham and Young Deuk Choi
Background
This study included a network meta-analysis of evidence from randomized controlled trials (RCTs) to assess the therapeutic outcome of transurethral resection (TUR) in patients with non-muscle-invasive bladder cancer assisted by photodynamic diagnosis (PDD) employing 5-aminolaevulinic acid (5-ALA) or hexylaminolevulinate (HAL) or by narrow band imaging (NBI).
Methods
Relevant RCTs were identified from electronic databases. The proceedings of relevant congresses were also searched. Fifteen articles based on RCTs were included in the analysis, and the comparisons were made by qualitative and quantitative syntheses using pairwise and network meta-analyses.
Results
Seven of 15 RCTs were at moderate risk of bias for all quality criteria and two studies were classified as having a high risk of bias. The recurrence rate of cancers resected with 5-ALA-based PDD was lower than of those resected using HAL-based PDD (odds ratio (OR) = 0.48, 95 % confidence interval (CI) [0.26–0.95]) but was not significantly different than those resected with NBI (OR = 0.53, 95 % CI [0.26–1.09]). The recurrence rate of cancers resected using HAL-based PDD versus NBI did not significantly differ (OR = 1.11, 95 % CI [0.55–2.1]). All cancers resected using 5-ALA-based PDD, HAL-based PDD, or NBI recurred at a lower rate than those resected using white light cystoscopy (WLC). No difference in progression rate was observed between cancers resected by all methods investigated.
Conclusions
The recurrence rate of some bladder cancers can be decreased by the implementation of either PDD- and NBI-assisted TUR; in real settings, clinicians should consider replacing WLC as the standard imaging technology to guide TUR.
Key Outcomes8
- Previous RCT and meta-analyses including this network meta-analysis have proven PDD and NBI canenhance the diagnosis of bladder lesions, guide an adequate resection, and reduce tumor recurrence.
- Both NBI and PDD are superior to WLI for reducing cancer recurrence rates after TUR-BT.
- When TUR-BT is performed using PDD or NBI, the recurrence rate of NMIBC is reduced compared toWLI by at least 35%.

NBI was found to be a valid alternative to PDD regarding diagnosis of CIS and flat dysplasia10.
A prospective, nonrandomized, international multicenter study from Scandinavia analyzed the within-patient comparison of WLI, NBI, and PDD in the detection of CIS or flat dysplasia in a TURB setting.
NBI – REVIEW OF CLINICAL EVIDENCE 04
Narrow-band Imaging Digital Flexible Ureteroscopy in Detection of Upper Urinary Tract Transitional-Cell Carcinoma: Initial Experience9
Olivier Traxer, Bogdan Geavlete, S. Gil diez de Medina, Matilde Sibony, and Saeed M. Al-Qahtani
Purpose
To characterize the appearance of normal and malignant upper urinary tract lesion appearance under narrow-band imaging (NBI) using the new URF-V digital flexible ureteroscope (DFU), and to determine if NBI, when used in conjunction with white light (WL), could improve detection of malignancy.
Patients and Methods
NBI and WL were performed in 27 patients at our university teaching hospital, 14 with known cases of upper urinary tract transitional-cell carcinoma (UUT-TCC) as follow-up (group A), and 13 patients with first-suspicion of cancer (group B). Full renal collecting system examination was performed first under WL and then under NBI by a single urologist. Biopsies were taken from all detected lesions using the
biopsy forceps and sent for examination by a pathologist who was blinded to the gross description of the lesion. Pathology interpretations were then compared with the corresponding WL and NBI images. Holmium laser vaporization was performed for all apparent lesions.
Results
Subjectively, NBI significantly improved the endoscopic visualization of the tumors, providing a detailed description of their limits and vascular architecture. Objectively, five additional tumors (14.2%) in four patients, as well the extended limits of three tumors (8.5%) in three patients were detected by NBI when findings by WL imaging were considered normal.
Conclusion
This is one of the first reports regarding NBI for UUT-TCC. From this study, we recommend this technology as a valuable diagnostic method, because it considerably improves tumor detection rate by 22.7% compared with WL.
Key Outcomes9
- NBI has a higher diagnostic power for identifying upper urinary tract transitional-cell carcinoma (UUT-TCC) than WLI alone, objectively confirmed via histological analysis.
- NBI enables the urologist to determine the exact limits of tumors, thereby facilitating complete laservaporization.
- From 35 detected, pathology-confirmed transitional-cell tumors NBI exclusively diagnosed five additionaltumors (14.2%), and identified extended limits for another 8.5% of tumors.
- NBI improves the tumor detection rate by 23% compared with WLI.
- NBI seems to represent a valuable diagnostic technology for UUT-TCC, showing considerableimprovement in tumor visual accuracy as well as in the tumor detection rate.
INCREASE DETECTION, REDUCE RECURRENCE
References
- Sylvester et al. Intravesical bacillus Calmette-Guerin reduces the risk of progression in patients with superficial bladder cancer: a meta-analysis of the published results of randomized clinical trials. J Urol 2002; 168:1964–1970.
- Jichlinski et al. Fluorescence cystoscopy in the management of bladder cancer: a help for the urologist! Urol. Int. 2005; 74:97–101.
- Kang et al. Narrow band imaging-assisted transurethral resection reduces the recurrence risk of nonmuscle invasive bladder cancer: A systematic review and meta-analysis, Oncotarget. 2016 Nov 03.
- Li et al. Diagnosis of narrow-band imaging in non-muscle-invasive bladder cancer: A systematic review and meta-analysis, International Journal of Urology 2013; 20:602–609.
- Babjuk M. et al. EAU Guidelines on Non-muscle-invasive Bladder Cancer. European Association of Urology (EAU), paragraph 5.11.2, EAU Guidelines Office, March 2017.
- Bladder cancer: diagnosis and management NICE guideline. Published 25
February 2015, nice.org.uk/guidance/ng2, retrieved on 20 February 2017. - American Urological Association (AUA)/ Society of Urologic Oncology (SUO)Guideline: DIAGNOSIS AND TREATMENT OF NON-MUSCLE INVASIVEBLADDER CANCER: AUA/SUO GUIDELINE, https://www.auanet.org/common/pdf/education/clinical-guidance/Non-Muscle-Invasive-Bladder-Cancer.pdf, retrieved on 20 February 2017.
- Lee et al. A network meta-analysis of therapeutic outcomes after new image technology-assisted transurethral resection for nonmuscle invasive bladder cancer: 5-aminolaevulinic acid fluorescence vs hexylaminolevulinate fluorescence vs narrow band imaging, BMC Cancer 2015; 15: 566.
- Traxer et al. Narrow-band Imaging Digital Flexible Ureteroscopy in Detection of Upper Urinary Tract Transitional-Cell Carcinoma: Initial Experience, J Endourol. 2011 Jan;25(1):19-23.
- Drejer et al. Comparison of White Light, Photodynamic Diagnosis, and Narrow-band Imaging in Detection of Carcinoma In Situ or Flat Dysplasia at Transurethral Resection of the Bladder: the DaBlaCa-8 Study. J. Urol 2017 Apr;102:138-142.
- Content Type