Maciej Gnass
MD, PhD

Prof. Artur Szlubowski
MD, PhD
Introduction
The collection of adequate material to allow cytological verification of a lung tumour when it is peripherally located is a challenge for the interventional pulmonologist. If the tumour is located very peripherally and there is no air-filled lung parenchyma separating it from the mural pleura, a relatively safe and effective option is to perform a transthoracic needle biopsy (transthoracic needle aspiration – TTNA) under ultrasound or computed tomography guidance, sometimes a trans-thoracic needle biopsy (TTNB). However, TTNA and especially TTNB performed through normal lung parenchyma carries a 15-25% risk of iatrogenic pneumothorax. Tumour biopsy performed with transbronchial access during bronchoscopy has a much lower risk of complications (<1% for pneumothorax). The main challenge is to delineate the biopsy site of lung tumour invisible in standard bronchoscopic examination.
Radial probe UM-S20-20R

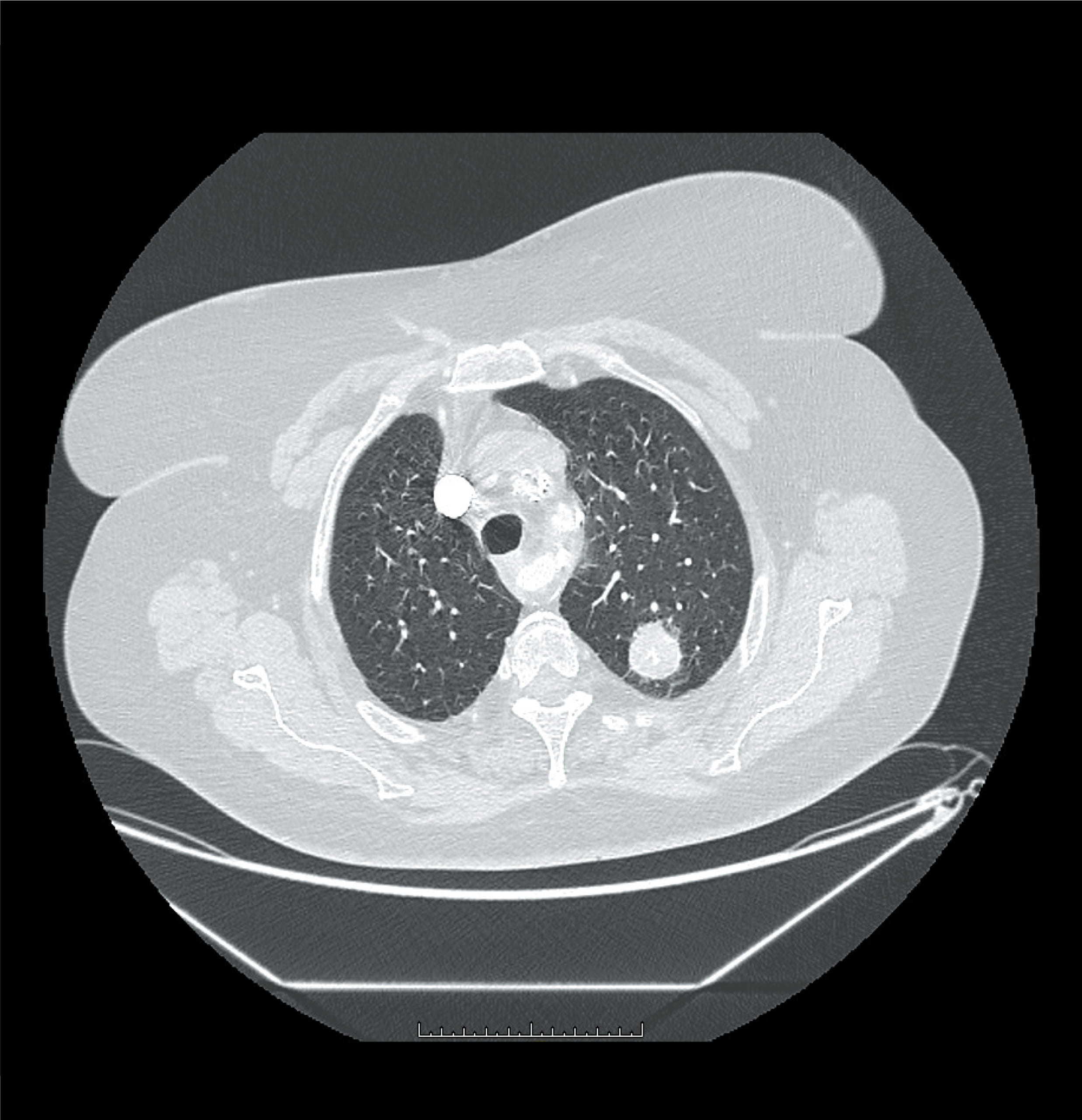
mage 1 shows a CT scan (lung window) with a solid nodule visible in the upper lobe of the left lung accessed by the posterior branch of the 3rd left bronchus.
The method of endobronchial navigation with an ultrasound-guided mini radial probe (UM-S20-20R) proposed by Olympus was introduced in our endoscopy laboratories (Krakow and Zakopane) in 2014. After a short time of testing, a full set with a GuideSheath and biopsy forceps, we decided to simplify and shorten the duration of the examination by resigning from the GuideSheath and markers of the distance of the lesion’s position in relation to the beginning of the endoscope’s working channel. We decided that it would be more precise to determine the distance of the tumour from the last sub-segmental ostium
visible in the bronchoscopic examination using metal rings visible on the radial probe. This method allows to locate the biopsy site and, what is important, eliminates the problem of possible displacement of the GuideSheath during breathing movements or coughing of the patient, as it allows to precisely determine the depth at which the tumour is located in a particular subsegmental bronchus. We have also made modifications to the biopsy tool, increasingly using a needle instead of forceps. In our opinion, the needle provides better penetration of the tumour, especially in the case of its peri-bronchial location. Thanks to the development of the method of preservation and evaluation of cytological material in the form of so-called cytoblocks, fine-needle biopsy allows us to perform most of the pathomorphological examinations as for the small biopsies obtained with the forceps method.
Cytological brush smears are performed occasionally, in selected cases and as an adjunct to needle biopsy, when the lesion is located tangentially to the examined bronchus (it does not end in the tumour or is not infiltrated by it in a circular fashion). In this situation, there is a risk that the biopsy needle in the long axis of the bronchoscope probe may not collect adequate material.
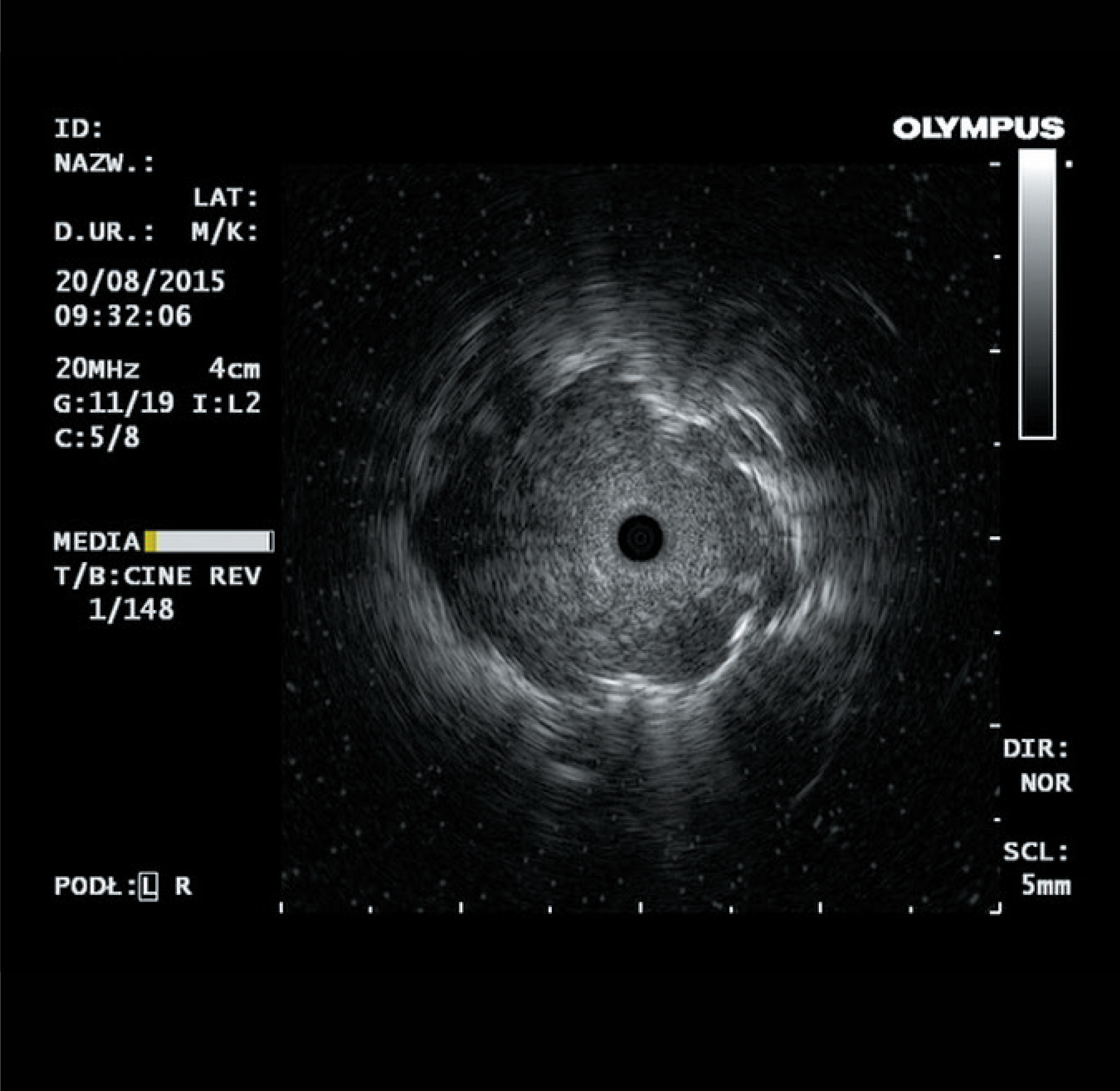
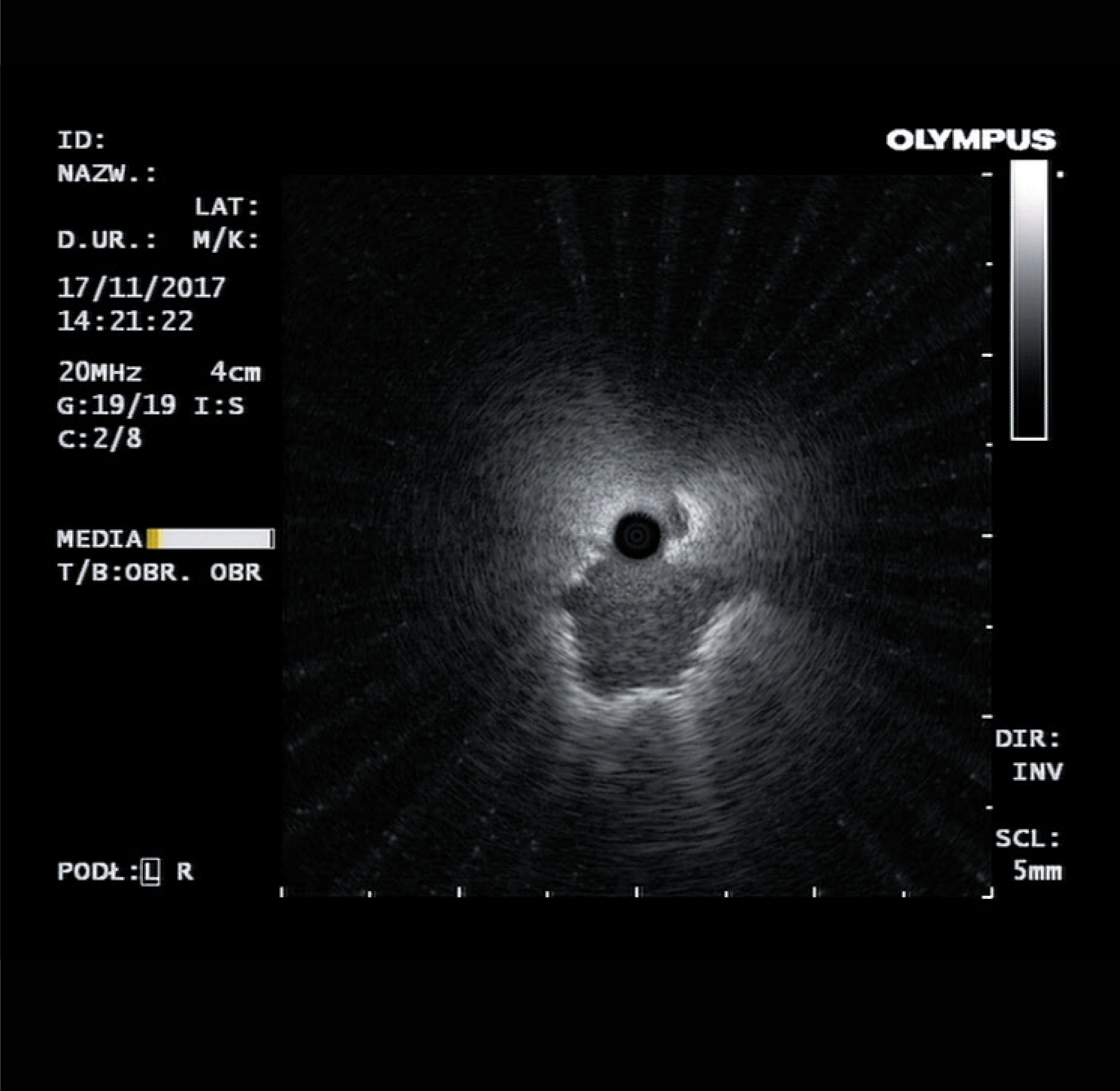
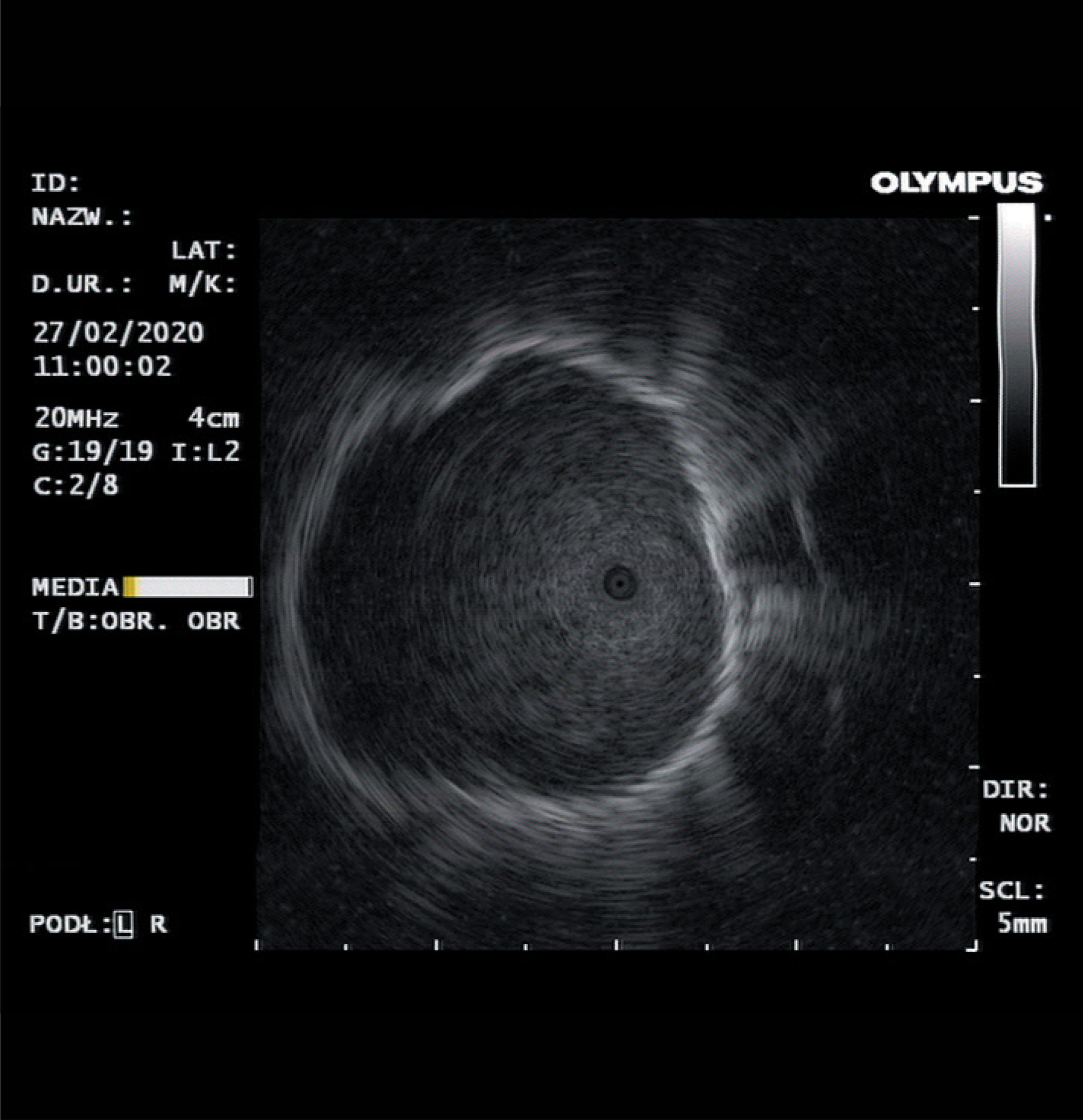
Image 2 shows two locations of the lung tumour in the radial probe image: a/the afferent bronchus in the centre of the tumour and b/the tumour located tangentially to the afferent bronchus.
If for some reason there are indications to collect more tissue material (tissue biopsy), we consider transbronchial cryobiopsy, also navigated by ultrasound-guided radial probe, to be the method of choice. We have therefore abandoned the use of biopsy forceps in the diagnosis of peripheral lung lesions.
After analysing a group of 107 patients with peripheral lung tumours diagnosed at the Krakow centre in 2015, we found a 75% sensitivity and 97% specificity of the method we use (rEBUS-TBNA).
At both centres, we perform a total of approximately 150-200 examinations per year using the ultrasound mini-radial probe in the diagnosis of peripheral lung tumours. So far, almost eight years of experience in performing such examinations allows us to claim that the TBNA biopsy needle is the most suitable biopsy tool for peripheral lung tumours. With its help one can effectively and safely (!) perform cytological verification of peripherally located lung tumours. Both bleeding requiring endoscopic intervention and pneumothorax are considered very rare complications (<0.5%). With tissue biopsy (forceps, cryoprobe), the risk of complications increases, in our material it is <5%.
Another added value, after abandoning the GuideSheath, is the increased flexibility of the bronchoscope with the radial probe inserted into the working channel. This enables the examination of more difficultly accessible lung segments (upper lower (apical of upper and superior of lower lobe – 1R, 1/2L and 6R/L). In order to reach the subsegments of these bronchi, bronchoscopes with a slightly smaller probe cross-section and a working channel of 2.0 mm (BF P180/P190) allowing the use of the UM-S20-20S radial probe are particularly useful.
With the use of an ultra-thin bronchofiberoscope (BF-MP190F) and a radial probe (UM-S20-17S) it became possible to localise very unfavourably localised peripheral lesions, which require significant bending of the bronchoscope probe tip and to reach 4-6th generation of bronchi.
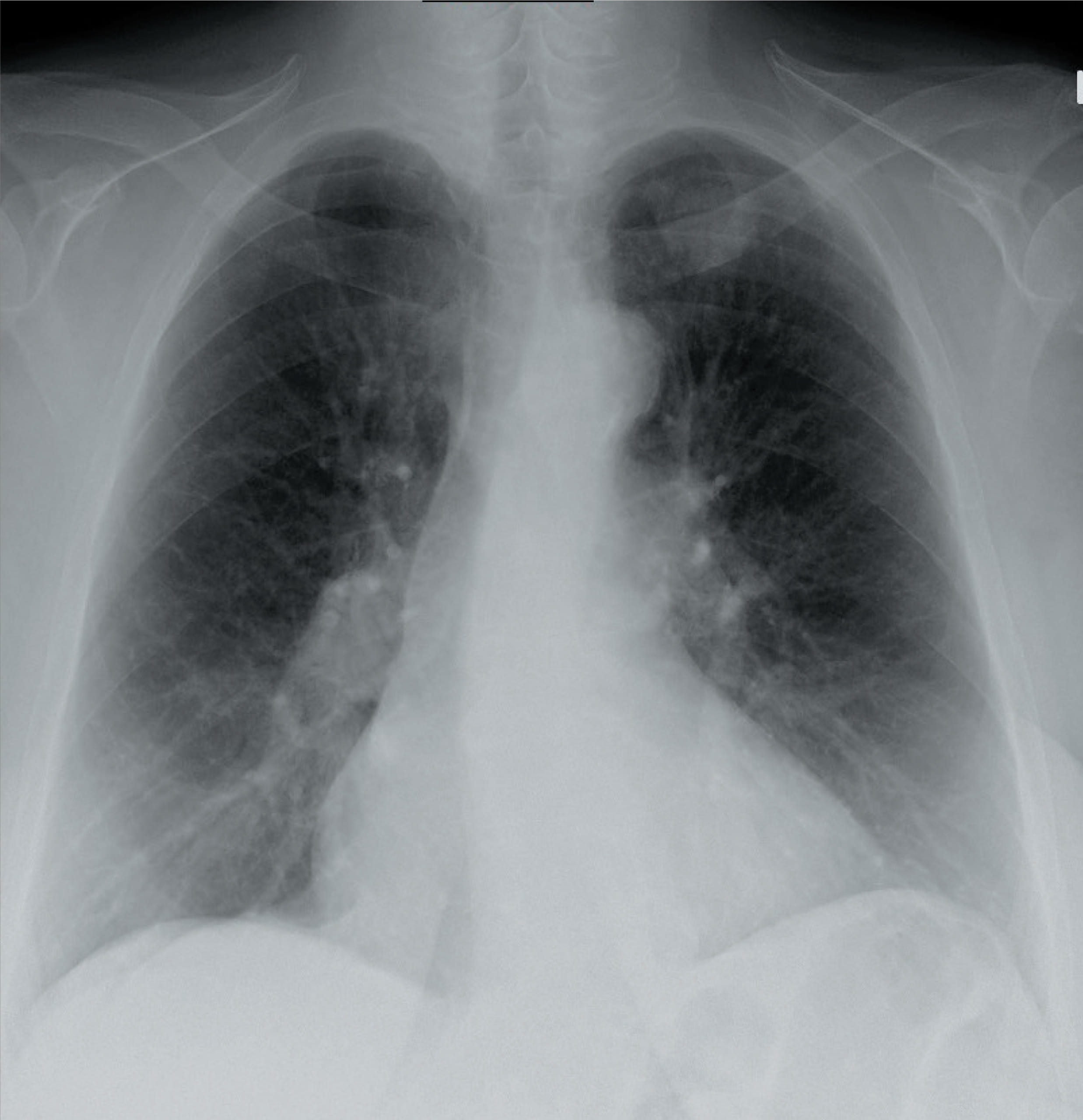
Image 3 shows an X-ray (a), a CT scan (b) and an image obtained with a radial probe (c) of a lung tumour located in the left lung apex.
While we are able to locate even very peripherally or unfavourably located lung nodules by endobronchial ultrasound, the problem is to find a suitable biopsy tool. It must be as flexible as a radial probe so that it does not stiffen the tip of the bronchoscope and can be introduced exactly into the place of the localized lesion.
PeriView Flex
The TBNA PeriView FLEX biopsy needle proposed by Olympus meets these conditions. Before the introduction of this needle into our practice, a problem arose in that, although a peripheral lung lesion could be localized (whether with a standard BFT180/190 bronchofiberoscope or an ultra-thin device), insertion of a standard TBNA needle, forceps or a cryoprobe into the target bronchus (recently, very flexible cryoprobes with a diameter of 1.1 mm have become available and first experiences with them have been positive in the discussed situations) proved to be impossible. The only available option in this situation was to perform a brush swab (this is a sufficiently flexible tool), which however rarely provides sufficient material for cytological examination.
The PeriView FLEX needle is therefore successfully used in cases requiring access to lesions located in segments 1/2L, 1R, 6R and 6L both in combination with a bronchoscope with a working channel of 2.8mm, 2.0mm and an ultra-thin bronchoscope with a channel of 1.7mm. In the case of the patient with a left lung nodule shown in the pictures 3a-c, the diagnosis of adenocarcinoma of the lung was made with the ultra-thin bronchoscope, radial probe and PeriView FLEX needle. The described needle in most cases allows to obtain material for fixation both in the form of cytoblocks and smears. In this it does not differ from other TBNA needles we have used so far and this seems to be mainly related to the structure of the biopsied tumour. This is important as one of the important indications for cytological verification of a lung nodule, especially in oncological patients, is an attempt to answer the question whether we are dealing with a primary lung lesion or a metastasis, as this implies the way of further treatment, including the extent of possible lung parenchyma resection.
Transbronchial biopsy of a peripheral lung tumour identified by ultrasonographic radial mini-probe appears to be an effective and safe method. Additionally, it is performed as an adjunct to standard bronchofibroscopy, which most patients with lung tumours have or will have performed. It also does not significantly prolong bronchoscopy and therefore does not require increasing doses of drugs used in analgosedation.
Skills development - sine qua non requirement
Its limitations are, apart from the localisation of the lesion (lack of the afferent bronchus in some cases makes the localisation, and thus the biopsy of the tumour, impossible), a very high impact of the experience and skills of the person performing the examination. This concerns both the interpretation of images obtained from computed tomography of the chest, on the basis of which the choice of examined lung segments is made, and spatial imagination, and above all, manual predisposition. It seems that to maintain high efficiency of the described method, a trained endoscopist should perform at least 50 procedures annually.
Apart from a perfect mastery of the technique of bronchoscopy, a large number of radial probe examinations is required for successful performance of such procedures. The interpretation of ultrasound image is usually not a problem, but more important is the macroscopic diagnosis, whether the material obtained during biopsy is suitable for cytological examination. Here, cooperation with a cytodiagnostician and/or pathomorphologist, from whom we can quickly (i.e. with the macroscopic image of the biopsy still in mind) and precisely obtain information whether the biopsy material is diagnostic, plays a fundamental role. In the era of molecular studies, not only the material containing tumour cells will be considered diagnostic, but also whether it will be possible to perform immunohistochemical or predictive tests.
Conclusions
As the purchase of endoscopic ultrasound equipment (processor, drive and radial probes) is a considerable expense, it seems reasonable to promote the implementation of this technique in pulmonology centres of II or III reference level, where many patients with lung tumours are seen and where decisions on further management are taken during oncology consultations. The large number of examinations performed ensures both an adequate level of experience of endoscopists and financial profitability of the purchase of equipment.
It would also seem most advisable to encourage endoscopists involved in minimally invasive staging of lung cancer using EBUS and EUSb, i.e. with ultrasound processors and experience, to acquire the skills to perform transbronchial biopsy of peripheral lesions. As mentioned above, this method is relatively simple, safe for the patient, and in clinical situations where tumour verification is necessary, it is a recommendable alternative to transthoracic biopsy, still the most popular in Polish conditions. Apart from the mentioned lower risk of iatrogenic pneumothorax, it does not cause the patient additional stress of another medical procedure (it is performed under analgosedation as an adjunct to routine pneumothorax) and does not charge the hospital ward with additional costs.
Authors
Maciej Gnass, MD, PhD, Independent Endoscopy Unit, John Paul II Specialist Hospital in Cracow, Poland; Endoscopy Unit, Public Specialized Hospital of Lung Diseases in Zakopane, Poland.
Professor Artur Szlubowski, MD, PhD, Independent Endoscopy Unit, John Paul II Specialist Hospital in Cracow, Poland; Endoscopy Unit, Public Specialized Hospital of Lung Diseases in Zakopane, Poland.
- Keyword
- Content Type