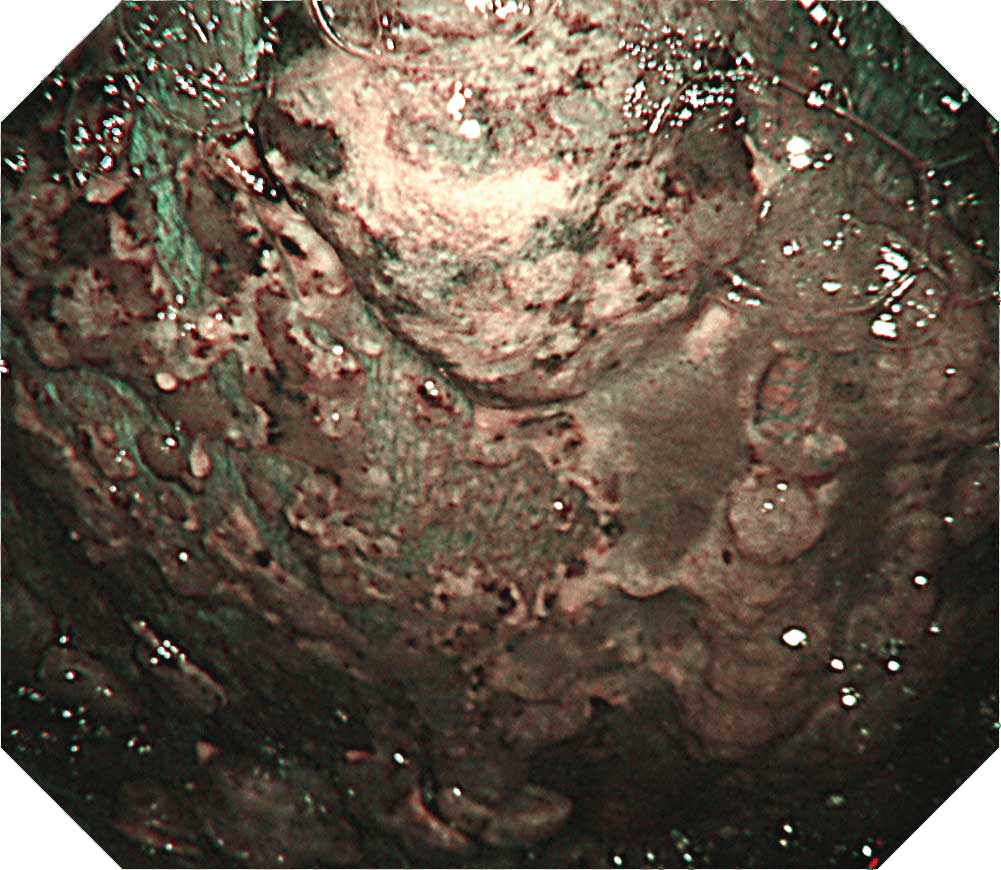
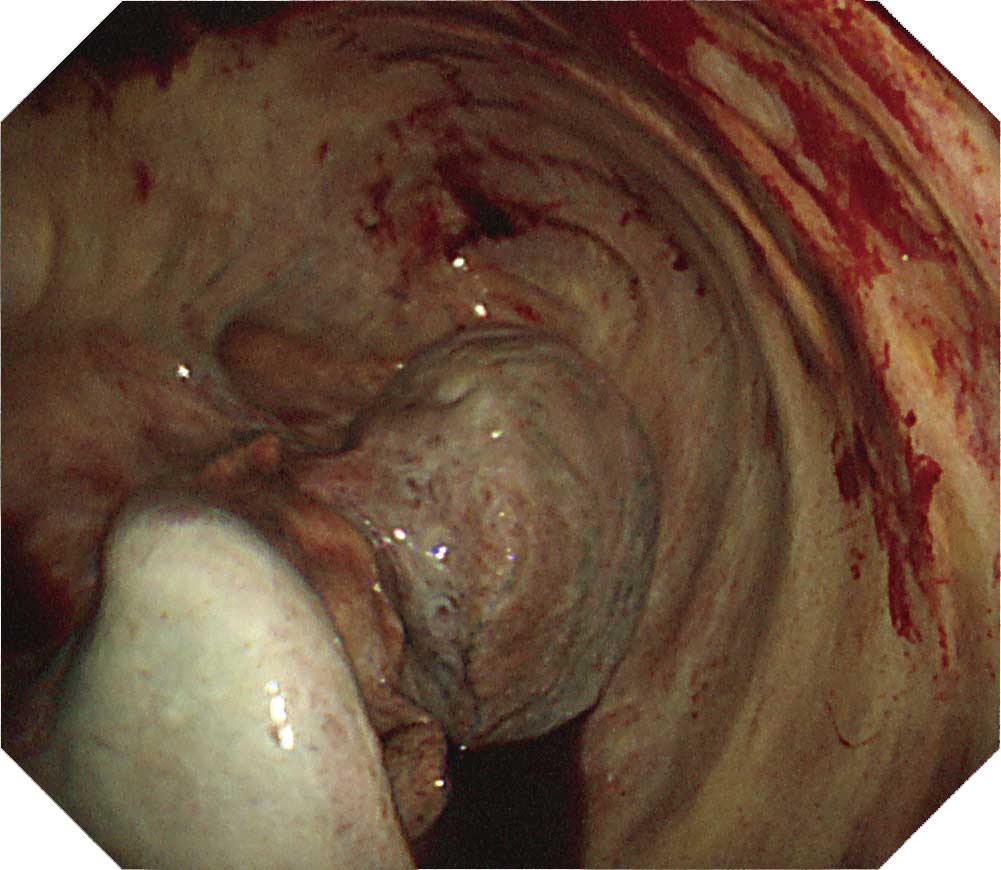
Malignant pleural mesothelioma
Takayuki Kaburagi — Ibaraki Prefectural Central Hospital and Cancer Center
Tip
When inserting the scope into the entry port, watch for chest wall thickening. Lesions on the visceral pleura often thicken to a degree that may prevent you from observing existing vessels and intercostal structures. There are also cases in which observation with thoracoscopy under local anesthesia is difficult due to pleural adhesion and formation of fibrous septa. When protruded lesions in this region reach a size between 5-10 mm, adjacent tumors may cluster and adhere to them. Dilated irregular vessels are often recognized in the tumor, while congested vessels are often recognized on the pleural surface. Pleural plaques which suggest asbestos exposure are confirmed in about half the cases. Ideally, all layers of the parietal pleura should be collected when performing a biopsy.
Acute empyema and nonspecific pleuritis
Akihiro Takemasa — Dokkyo Medical University
Tip
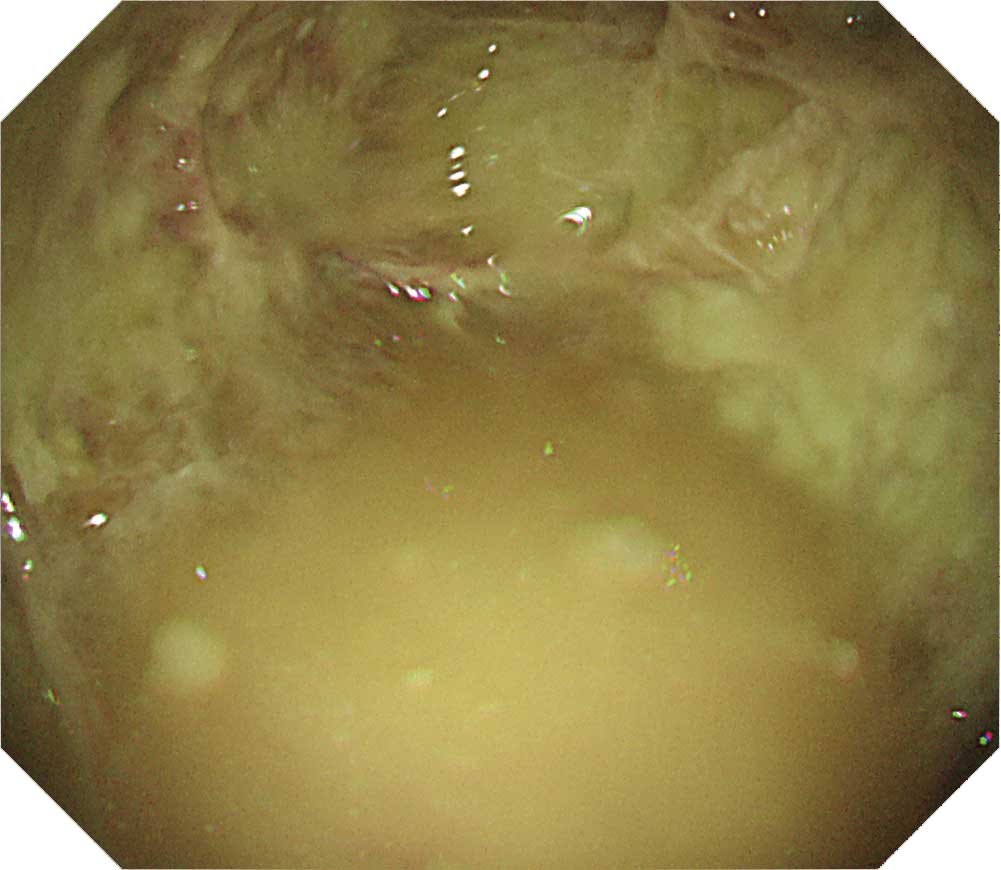
Acute empyema (H-1, 2, 3):
With acute empyema, compartments tend to form rapidly due to fibrin deposition, which often makes it difficult to perform drainage. If the adhesion can be detached using a thoracoscope at as early a stage as possible, the range of effective drainage can be expanded, making it possible to shorten the treatment period.
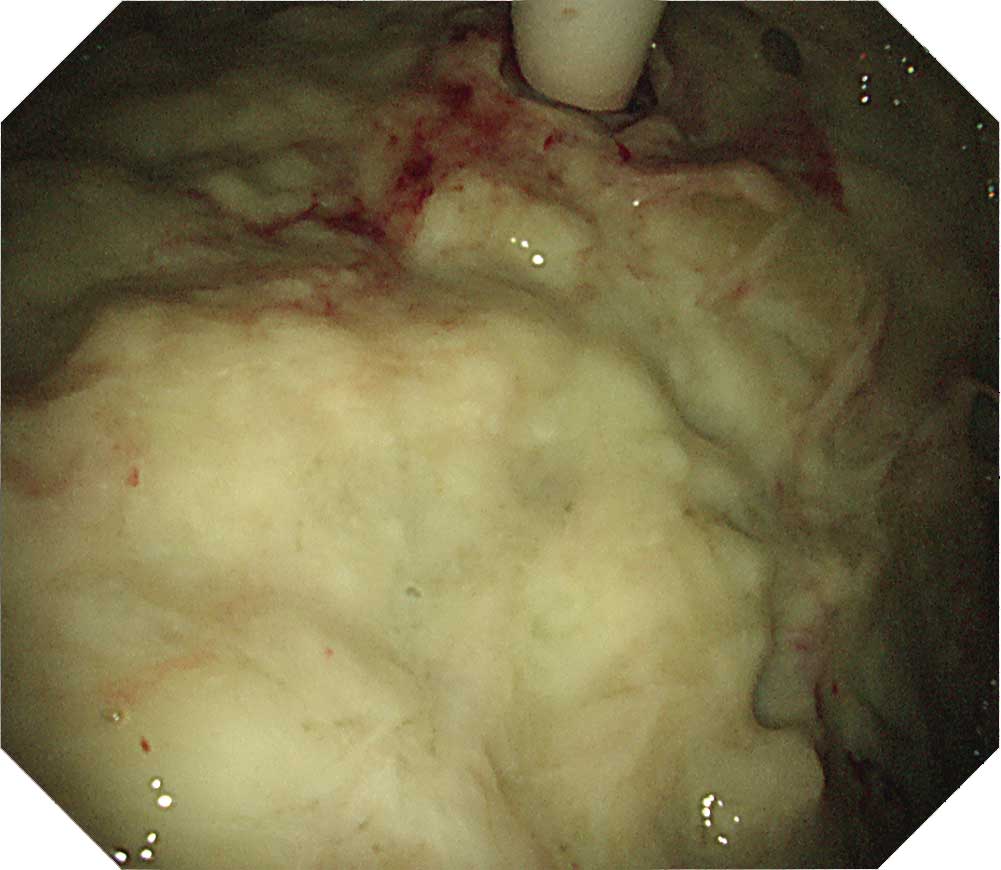
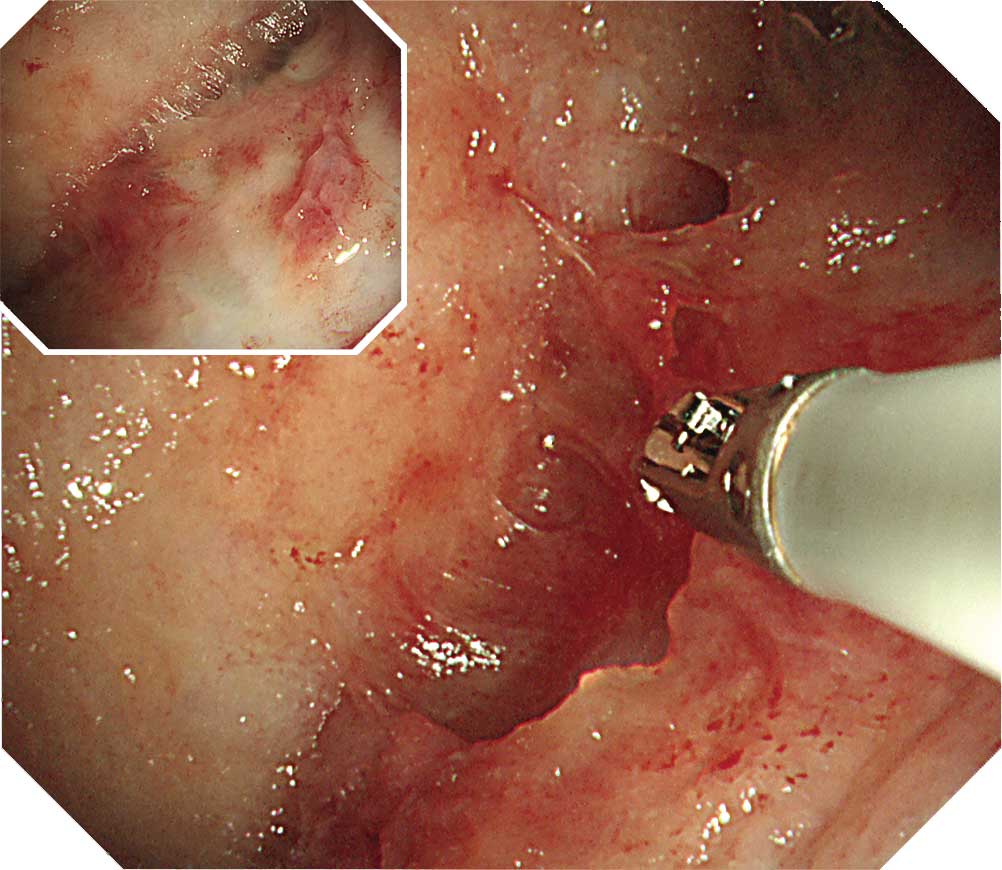
Nonspecific pleuritis (I-1, 2, 3):
A fibrinous adhesion manifested in nonspecific pleuritis is an adhesion attached by white sparse fibrin membrane and can easily be destroyed with forceps. When it turns fibrous from fibrinous and the adhesion becomes strong, the visceral and parietal pleurae will become inseparable.
Nonspecific pleuritis and chronic fibrous pleuritis
Akihiro Takemasa — Dokkyo Medical University
Case J-1: Nonspecific pleuritis case with a history of asbestos exposure
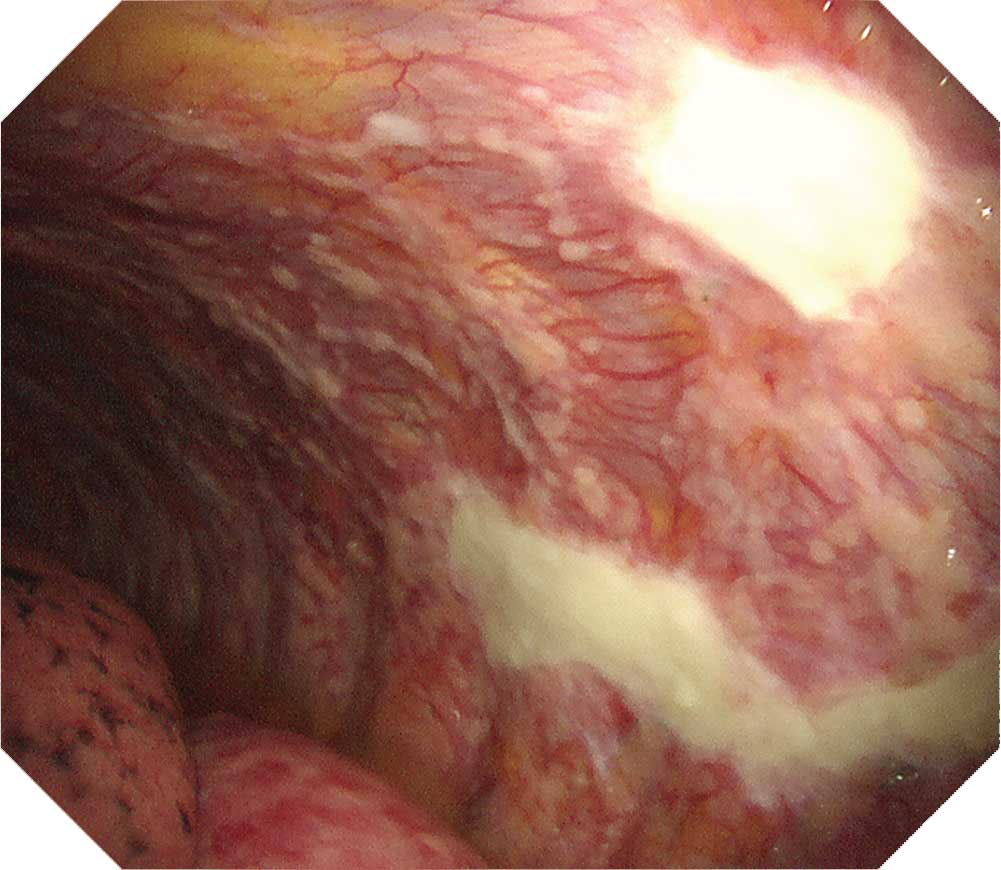
The parietal pleura decreases the visibility of the intercostal muscles and vessels. The intercostal depressions also decrease, which obscures the intercostal spaces. The resulting image shows the moderately thickened pleura. The visceral pleura is covered with a white fibrin membrane, preventing the lung from expanding (trapped lung).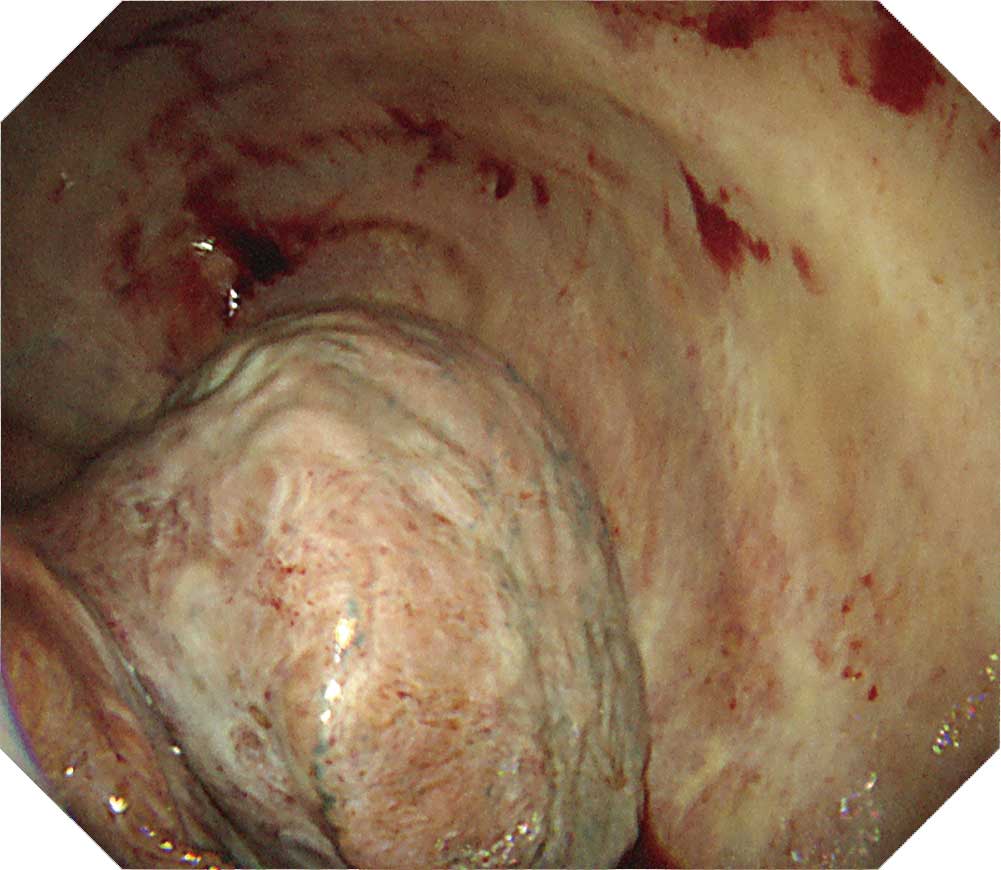
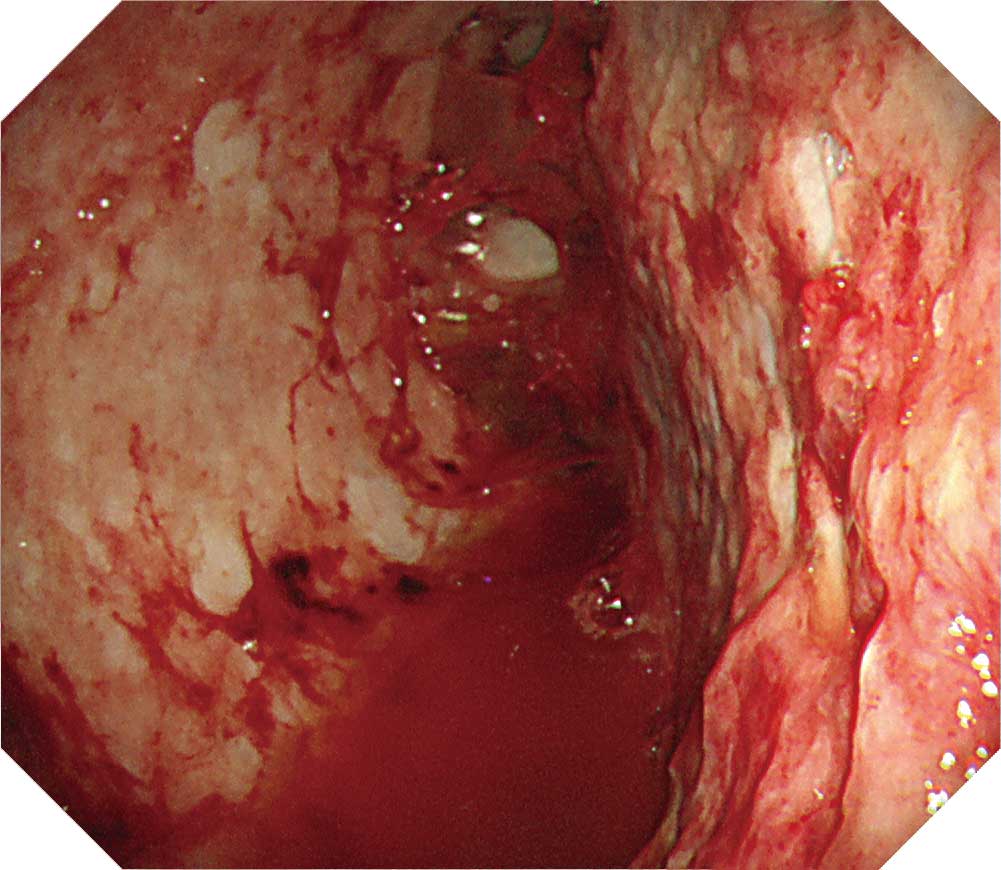
Case J-3: Nonspecific pleuritis case with a history of asbestos exposure
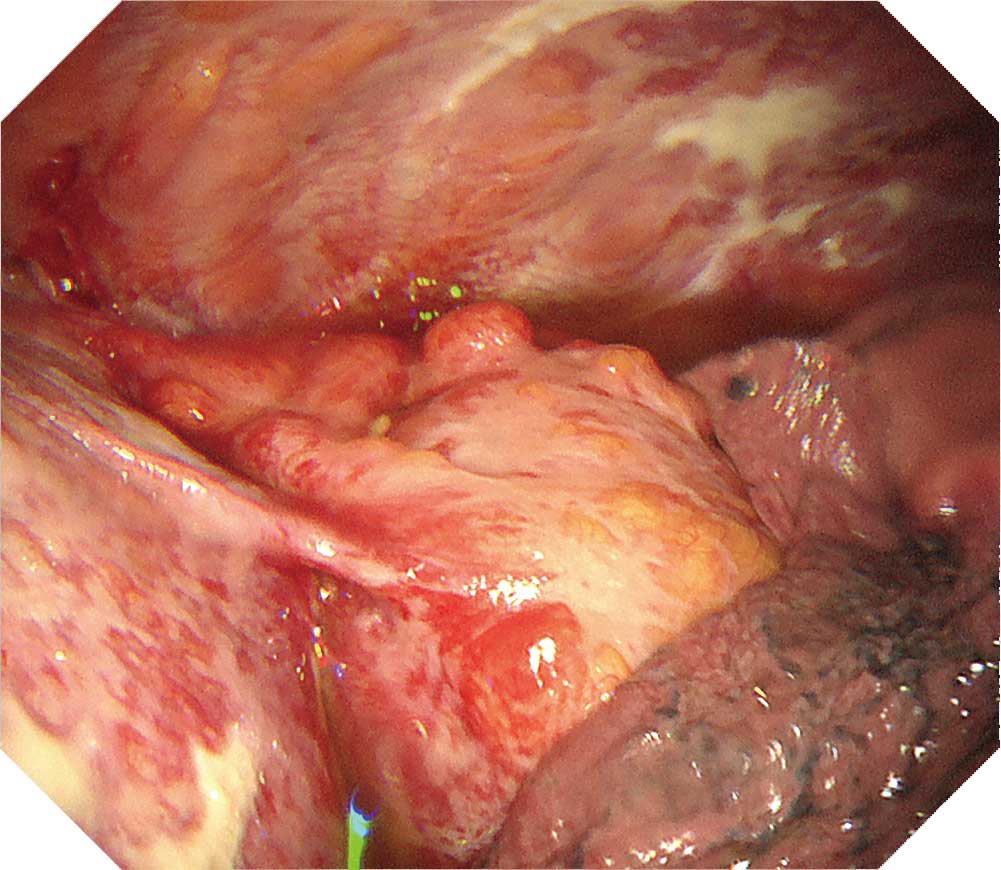
Part of the visceral pleura exhibits severe pleural thickening, making it impossible to view any of the structures such as the intercostal muscles and vessels at all. The visceral pleura is also thickened, obscuring the structures on the surface of the lung.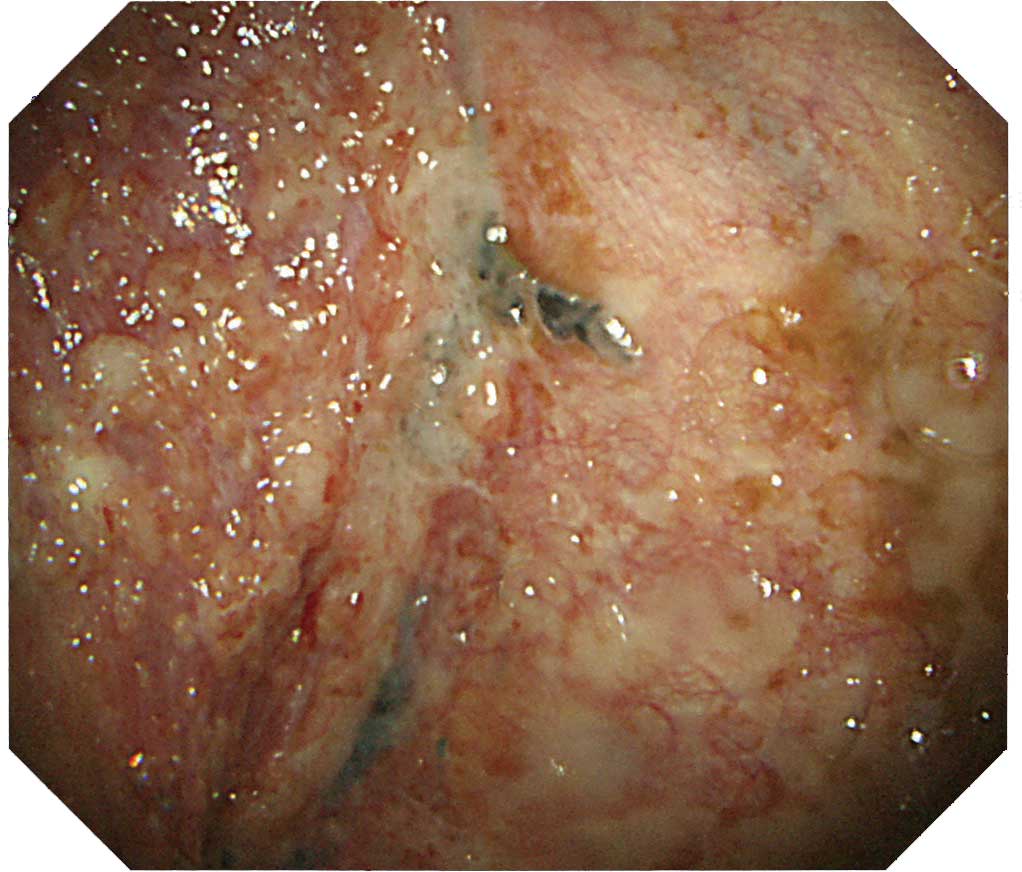
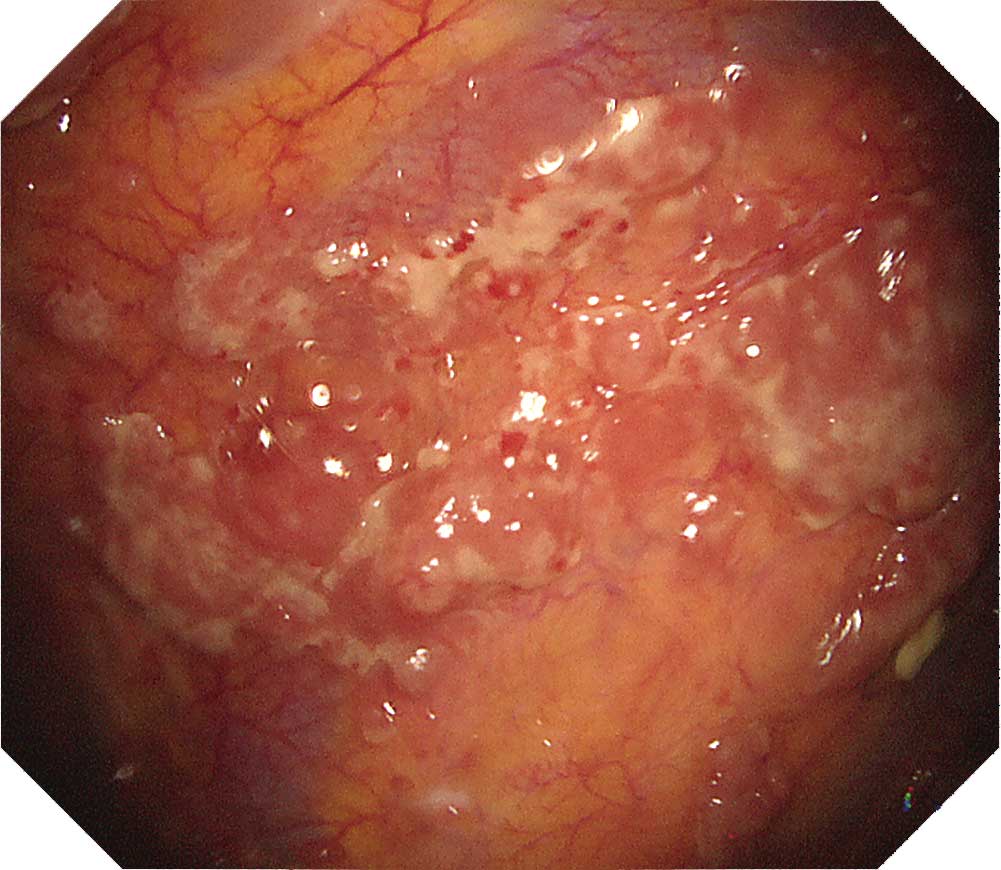
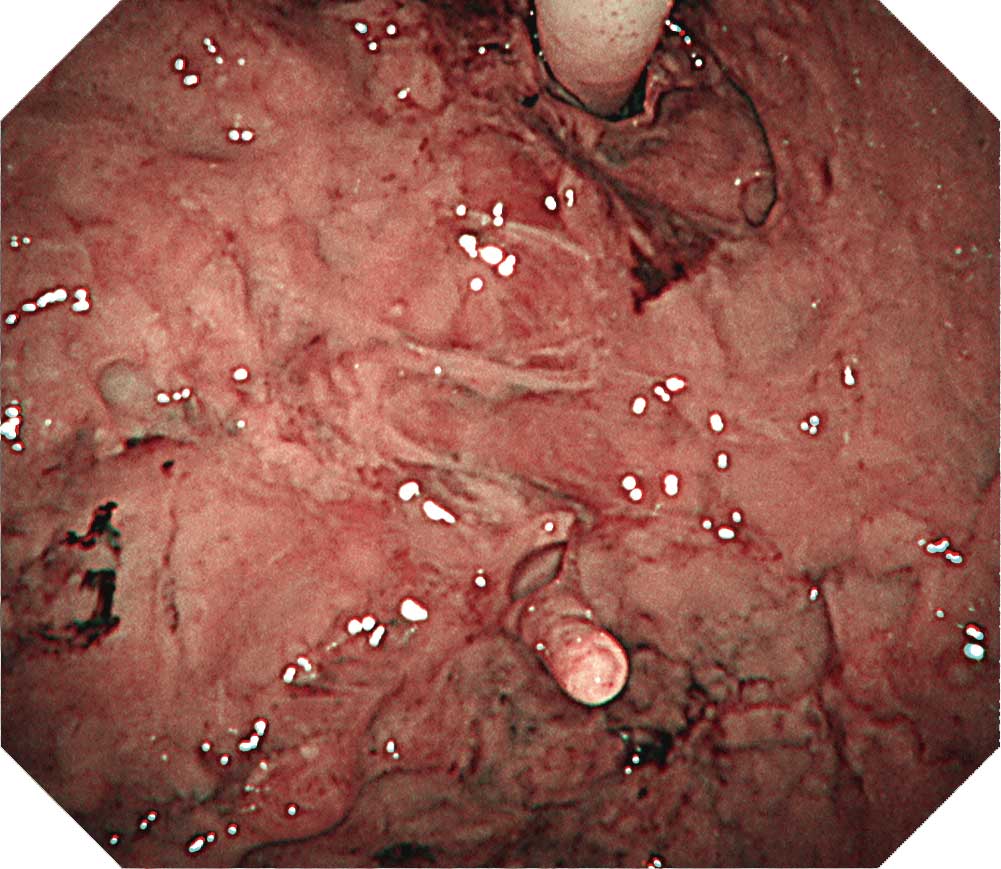
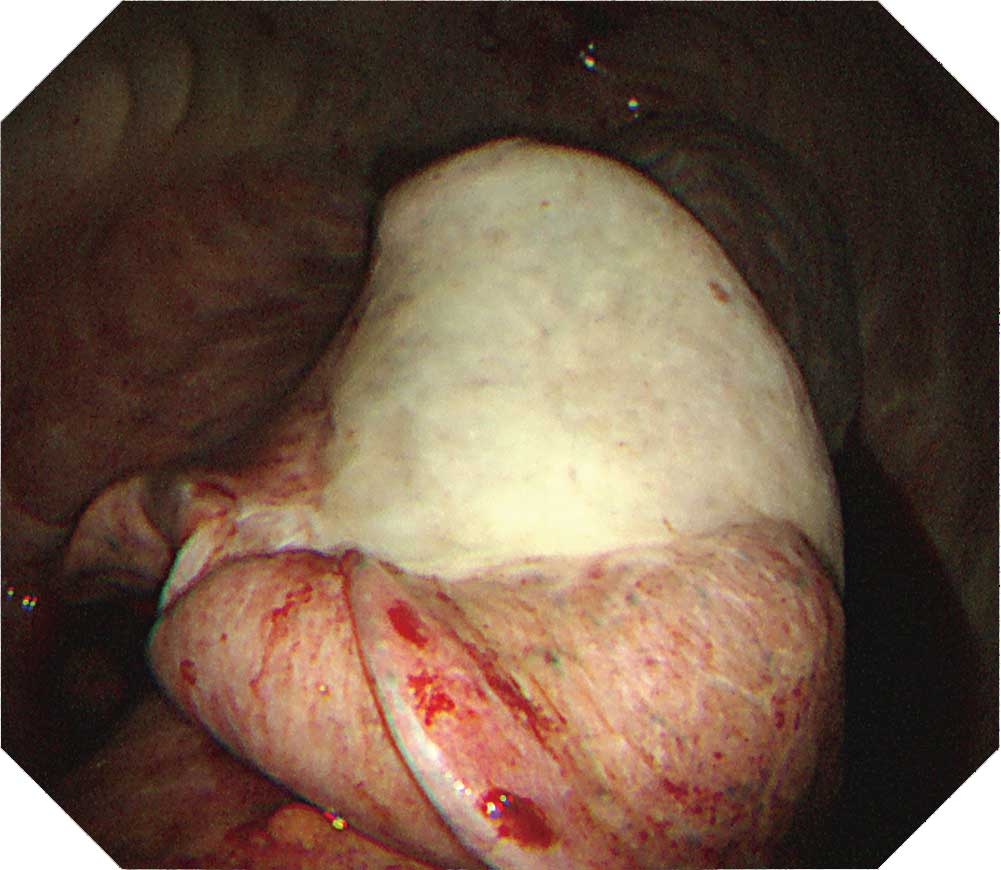
Case K-2: Chronic fibrous pleuritis case with a history of asbestos exposure
Recognized here are pleural thickening and multiple occurrence of granular lesions on the surface. We performed full-thickness biopsy using both an electrosurgical knife and cryobiopsy device but did not detect any invasion of mesothelial cells into the fat layer, leading us to diagnose this case as chronic fibrous pleuritis.
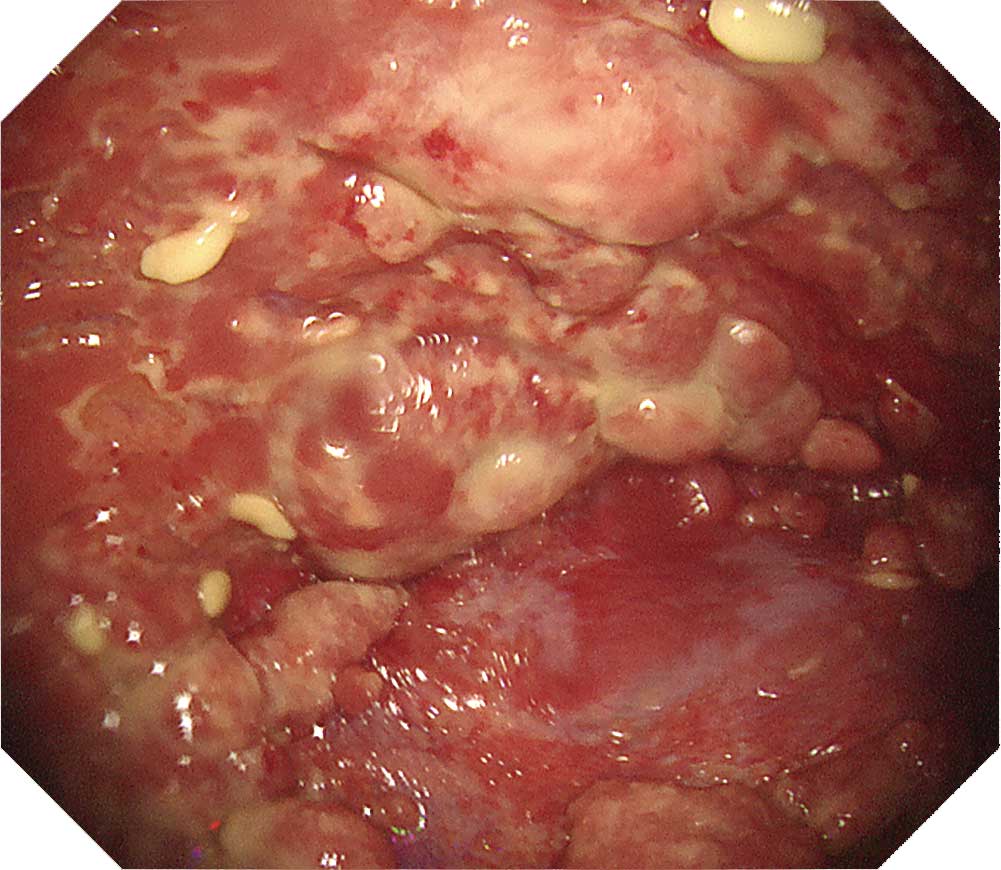
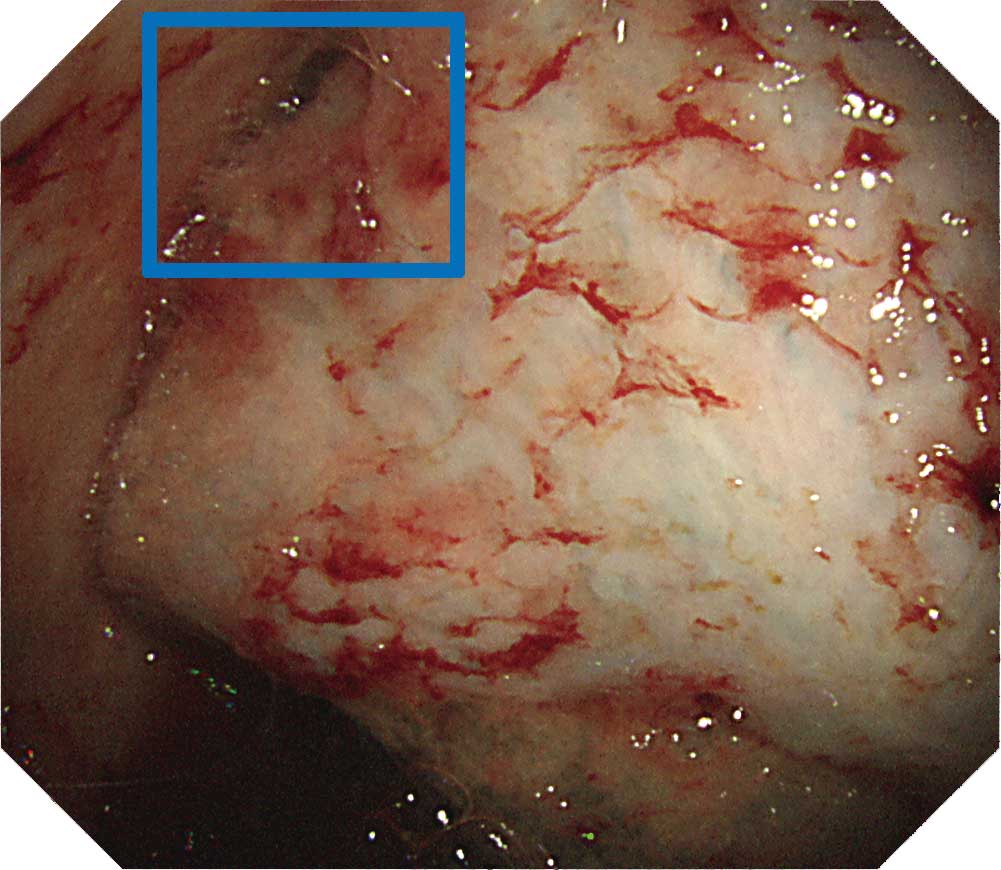
Case K-3: Chronic fibrous pleuritis case with a history of asbestos exposure (NBI image)
There is a multiple occurrence of granular lesions on the surface of the thickened pleura. In this NBI image, dilated vessels can be recognized in some parts; however, most parts are covered with white fibrous coating.Tip
Nonspecific pleuritis (J-1, 2, 3) and chronic fibrous pleuritis (K-1, 2, 3):
Both cases have a history of asbestos exposure. Complications in such cases may include trapped lung, candle wax spots, and pleural plaques. Protrusions typically seen in malignant tumors may also be recognized. In cases such as these, a full-thickness biopsy can be a decisive means of diagnosis. Depending on the case, the use of an electrosurgical knife and cryobiopsy device should be considered as and when required.
- Content Type