Intact Papilla : Post-gastrectomy Roux-en-Y, Post-choledochectomy Roux-en-Y, and Billroth-II

Takao Itoi, MD, PhD, FASGE
Department of Gastroenterology and Hepatology,
Tokyo Medical University

Ryosuke Tonozuka, MD
Department of Gastroenterology and Hepatology,
Tokyo Medical University
Preparation
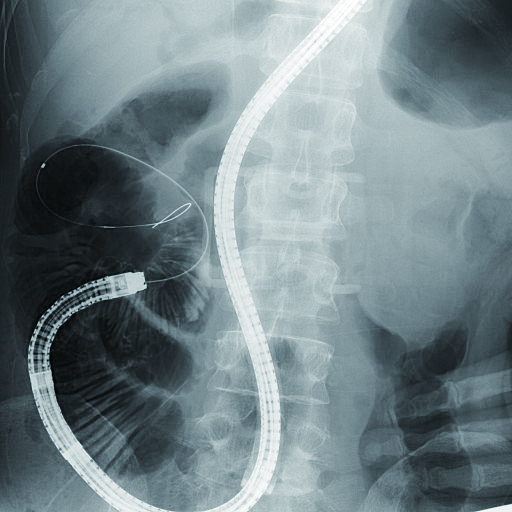
Before beginning the procedure, use fluoroscopy to clarify number/size of stones or location of stricture for preparing the appropriate endotherapeutic devices.
Regardless dealing with a Roux-en-Y (R-Y) anastomosis case or a Billroth-II (B-II) reconstruction case, it is important to collect as much pertinent information as possible beforehand. In the former case, you will need to know the length to Y-limb or anastomosis method performed on Y-limb (end-to-side or side-to-side), while in the latter case, you need to know performed gastrojejunostomy method (anterograde or retrograde) or the presence of Braun anastomosis.
Confirmation with fluoroscopy (for preparation of endotherapeutic devices)
- Size and number of stones
- Location of stricture
Confirmation with surgical method
R-Y case
- Length to Y-limb
- Y-limb anastomosis method (end-to-side or side-to-side)
B-II case
- Gastrojejunostomy method (anterograde or retrograde)
- Presence/absence of Braun anastomosis
Operation environment
・Equipment required (Fig. 1)
Whenever you perform short-type single balloon enteroscopy (sSBE), you will need SIF-H290S small intestinal videoscope, EVIS LUCERA ELITE video processor and light source compatible with the endoscope, ST-SB1S splinting tube for sSBE, and the OBCU balloon control unit.
Ideally, you should use CO2gas for endoscopic insufflation whenever possible. Before starting the procedure, you can mount a distal attachment on the tip of the endoscope beforehand.
・Sedation method and patient position
For sedation, we use pentazocine (Sosegon®) as an analgesic and flunitrazepam (Silece®) as a sedative.
As for patient position, we place patient in left lateral position for endoscope insertion and keep them in that position until endoscope reaching to gastrojejunal/esophagojejunal anastomosis or pylorus. Once past through those regions, we shift patient to prone position as this makes it easier to grasp endoscope position in fluoroscopy.



Insertion technique (anatomy, workflow and tips of insertion, selection of afferent limb, and tips on passing through bends)
1) Post-gastrectomy Roux-en-Y (RY) cases
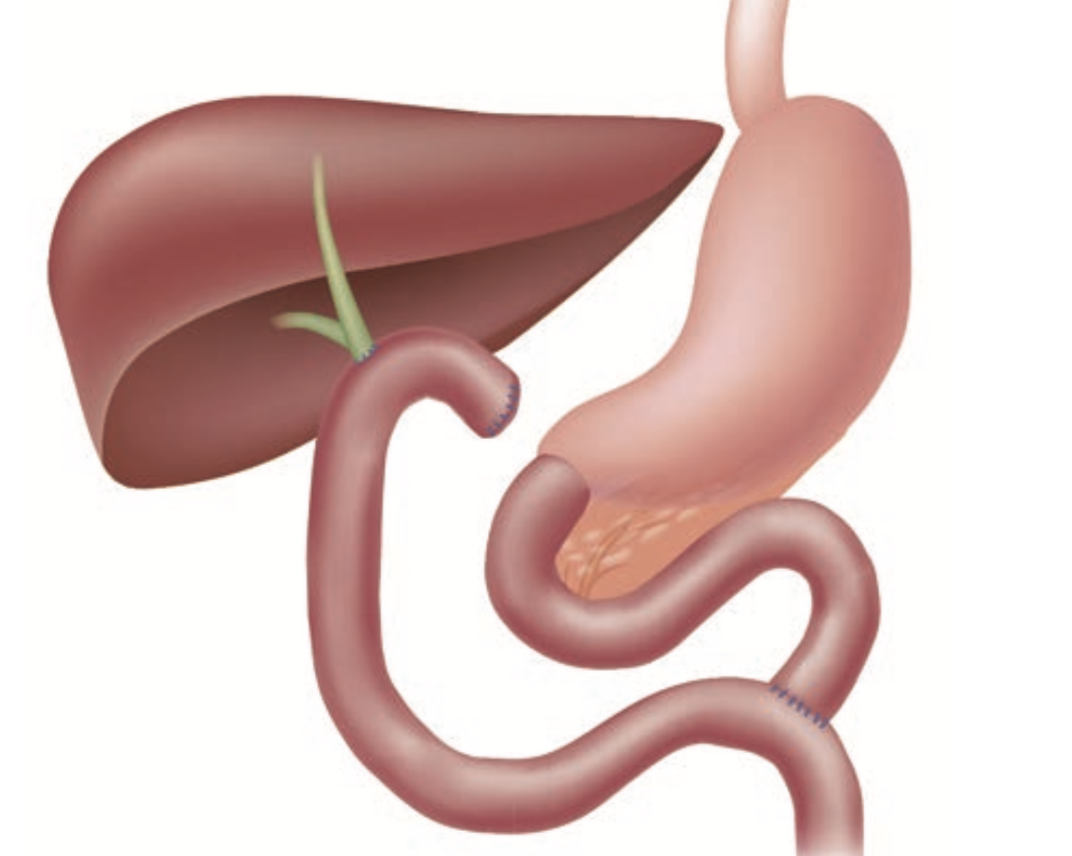
In terms of anatomy, the length from esophagojejunal anastomosis to Y-limb is about 30 cm when an operation is performed.
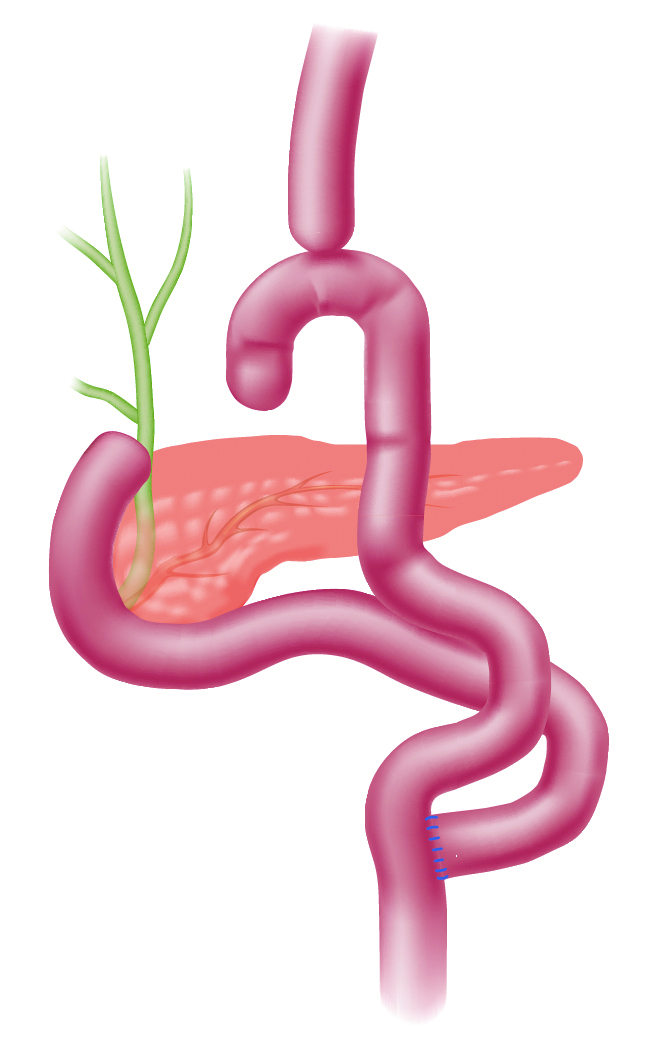
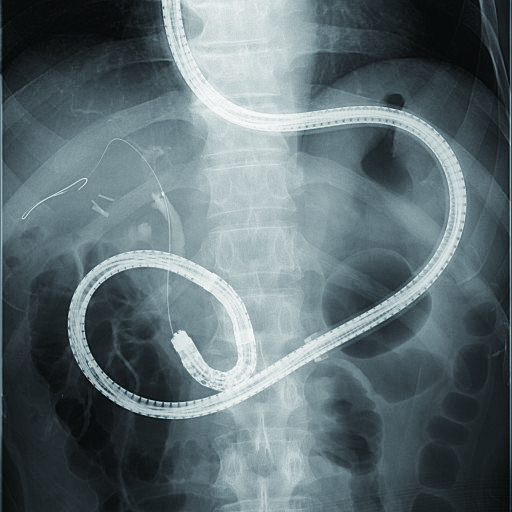
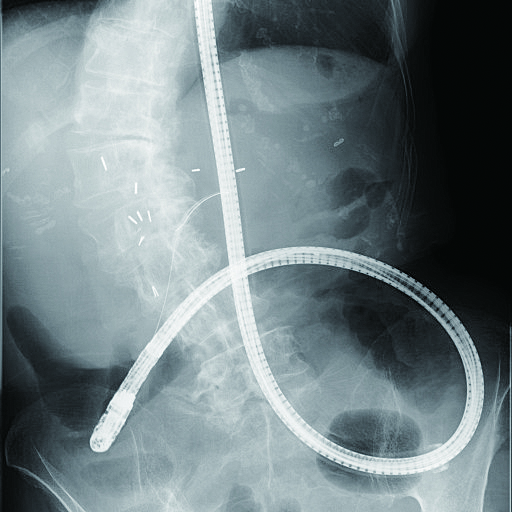
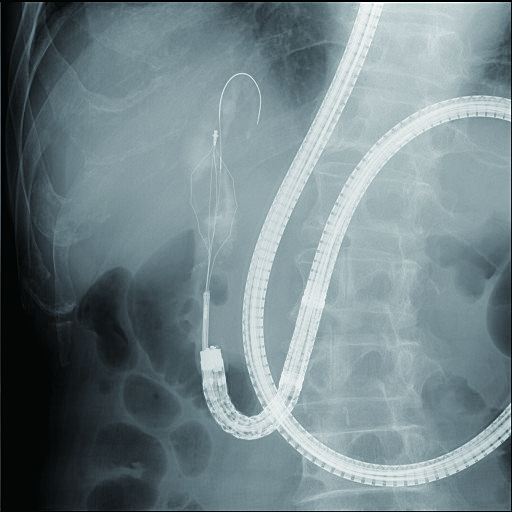
However, frequent pushing of endoscope during insertion can stretch the tract as much 60 cm or more. Alternatively, another Y-limb may be formed with a loop. You must repeatedly use tract shortening procedure to keep any extension of the tract to a minimum for finding a so-called “joint” where there are no jejunal folds or a large space (Fig. 2a) with fluoroscopic images (left lateral cranial direction).
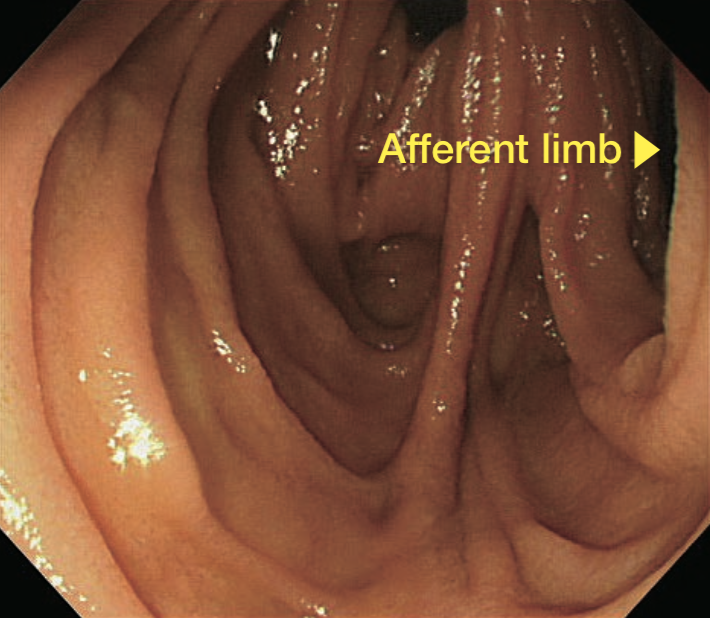
Generally, afferent limb is located in the tract (Fig. 2b) where endoscope tip is observed in the left lateral cranial direction under fluoroscopy. Insertion is usually more difficult at this point.
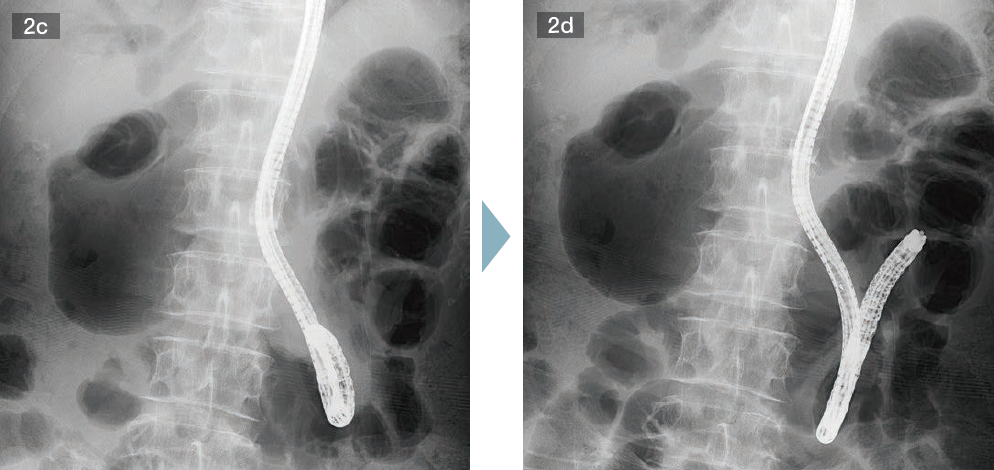
This leaves you with no option but to sharply bend endoscope tip to advance the endoscope. However, bends endoscope tip results in a shape that resembles a walking stick handle. If you keep pushing conventional endoscope in that condition, the endoscope axis will move toward efferent limb. Thus, even if the endoscope tip enters afferent limb, it will end up heading in the direction of efferent limb easily. However, SIF-H290S applied a couple of remarkable functions — Passive Bending and High Force Transmission — that makes it much easier to advance the endoscope to afferent limb with combination of simple pushing and downward angulation, compared to conventional endoscope (Figs. 2c, 2d).
If you still find it difficult to advance to afferent limb, you will find it helpful to: 1) apply manual compression from caudal side under fluoroscopic guidance; and 2) hit the endoscope tip against the opposite side to Y-limb by taking advantage of twisting of the endoscope when the angle is not so sharp. In a method like sSBE — in which splinting tube is advanced by taking advantage of hook formed at the endoscope tip — it is effective to advance the endoscope tip after advancing it as close to the blind end as possible.
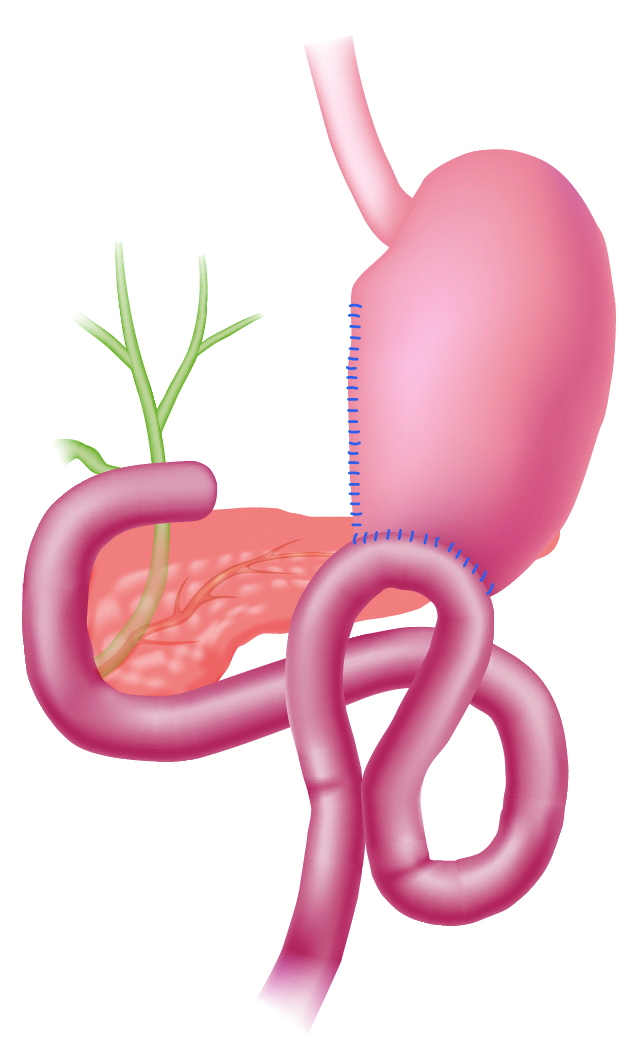
Illustration of post-gastrectomy R-Y reconstruction

2) Post-choledochectomy R-Y cases
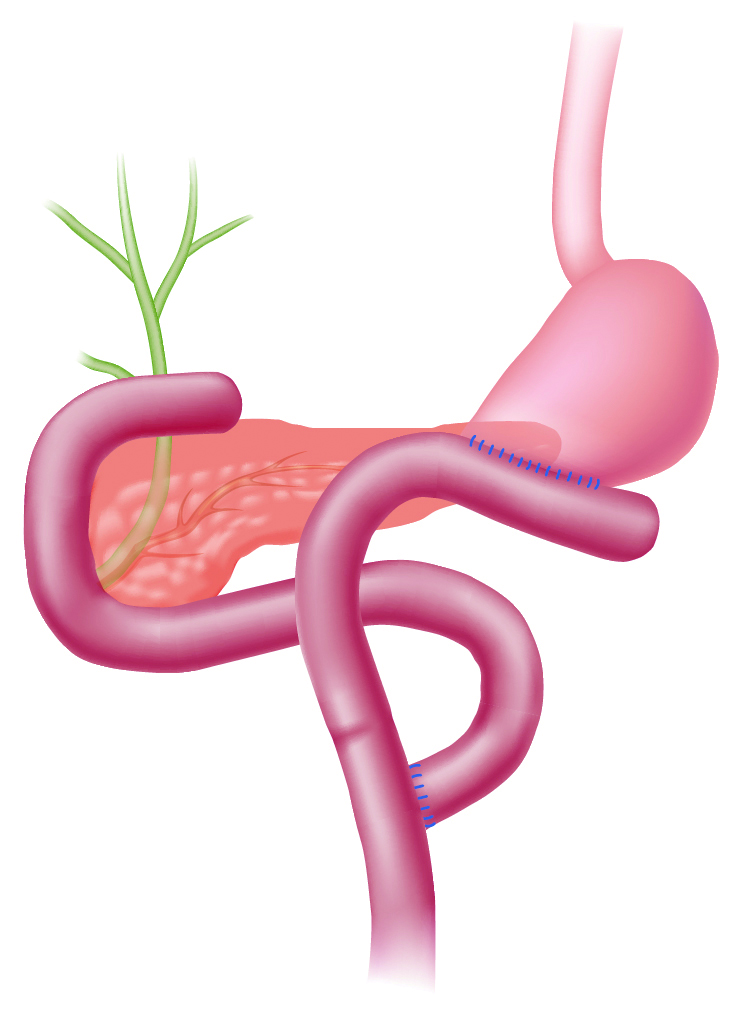
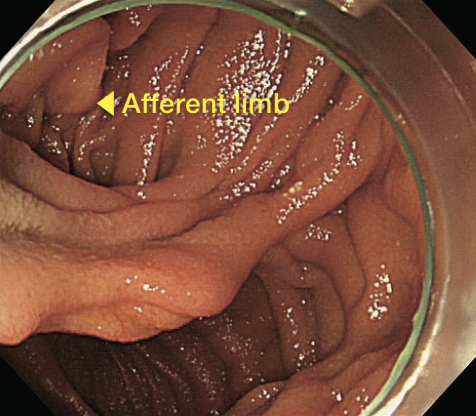
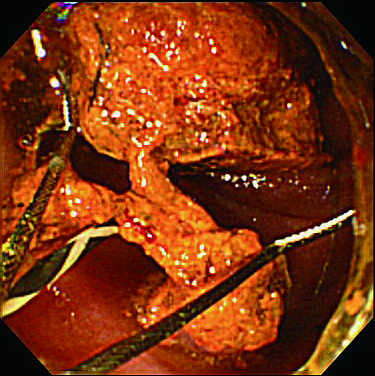
When performing a hepaticojejunostomy plus R-Y anastomosis after a choledochectomy, it is slightly more difficult to reach to the blind end of afferent limb than with a subtotal gastrectomy, a total gastrectomy plus R-Y anastomosis, or a post-pancreaticoduodenectomy. This is true even if a balloon enteroscope is used because of the length of endoscope that has to pass through stomach and duodenum. However, unlike anastomosis with total or subtotal gastrectomy, R-Y anastomosis performed in conjunction with a hepaticojejunostomy forms so-called “T-junction, which means that the angle of end-to-side anastomosis is not as sharp as anastomosis with total or subtotal gastrectomy. Consequently, afferent and efferent limbs are more often observed as two openings (Fig. 3a).
When advancing the endoscope to the afferent limb after the two openings have been observed, success rate is relatively higher when the endoscope is directed to luminal wall, which makes the endoscope tip point to the right and cranial side in fluoroscopy (Fig. 3b). However, this is not necessarily correct approach. Presence of bile also provides a useful guide as to which direction to choose in order to successfully advance the endoscope to afferent limb. Again, we must point out that this method, like the previous method, is not always correct.
Moreover, even if you succeed in advancing the endoscope to the afferent limb, you may find it difficult to advance it on the proximal side in the vicinity of hepaticojejunal anastomosis due to the presence of sutures or adhesion of elevated jejunum and colon (Fig. 3c). Should this be the case, insert splinting tube to as full extent as possible and change the patient position and/or apply hand pressure to advance the endoscope tip.

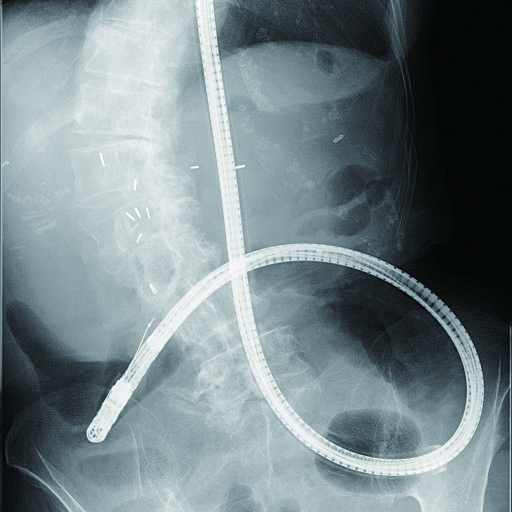
3) Billroth II (B-II) reconstruction case
Size of anastomosis depends on surgeon and varies greatly from case to case — such as when afferent and efferent limbs can clearly be recognized as two openings or when only one opening can be recognized. In many cases, afferent limb can be observed all the way from anastomotic opening. However, entrance to the efferent limb tends to form a sharp angle, often making it impossible to observe. Should that be the case, use the area around anastomotic site on the opposite side to folds on greater curvature of stomach as a reference point to look for slit-shaped entrance to efferent limb. When doing this, insert the endoscope tip into the slit while angulating the scope up towards lesser curvature, taking into account any subsequent maneuvering of endoscope. At this time, the distal end of the endoscope usually points to the right side of patient body (Fig. 4a). In addition, there are cases in which it may be useful to perform insufflation to create gaseous images in small bowel in order to confirm whether or not the site in question is afferent limb, as well as to measure the distance to remaining distance to the blind end.
Illustration of B-II
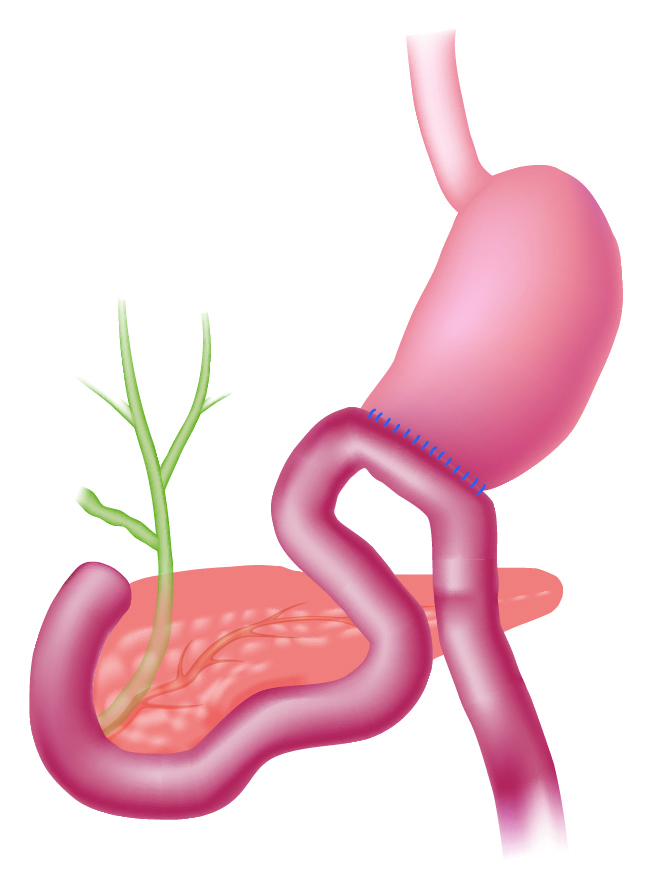
If the endoscope is angulated sharply upward even if distal end has already entered entrance to afferent limb, simply pushing the endoscope will not make it advance any further. Instead, you should pull the endoscope slightly to straighten shaft so that it is aligned with afferent limb while releasing upward angulation a little at a time. Now you can advance the endoscope by pushing it in (Fig. 4b).
In cases where Braun anastomosis is present, insertion may be difficult because the entrance to afferent limb at gastrojejunal anastomotic site is too steep. If so, you can also approach duodenal papilla via the Braun anastomosis after the endoscope is once inserted into efferent limb.

Tips on how to approach papilla
As opposed to ordinary ERCP, the endoscope is inserted from the anus, so that long axis of papilla is upside down. With a forward-viewing endoscope, it is basically impossible to get a frontal view of papilla in ordinary ERCP. As a result, in most cases — whether R-Y case or B-II case — observation in a tangential direction cannot be avoided. Nevertheless, so-called “J-turn” is often possible in B-II case (Fig. 4b). This allows a frontal view of papilla (although it is upside down). One of methods for obtaining a frontal view of papilla in R-Y cases is a technique called “retroflex position”. This involves performing cannulation with an endoscope position similar to J-turn while you push the endoscope slightly by intentionally retroflexing the endoscope tip near inferior duodenal flexure (Figs. 5a, 5b).1), 4) In some cases, it is not possible to adjust endoscope to retroflex position, which means that it may not be possible to obtain a frontal view of papilla depending on location of papilla, presence/absence of diverticula, and size of lumen. It is also important to keep in mind that while a mounted distal attachment can sometimes be useful during insertion as well as for fixing papilla and intubating into bile duct, it can also interfere with maneuvering of the endoscope.
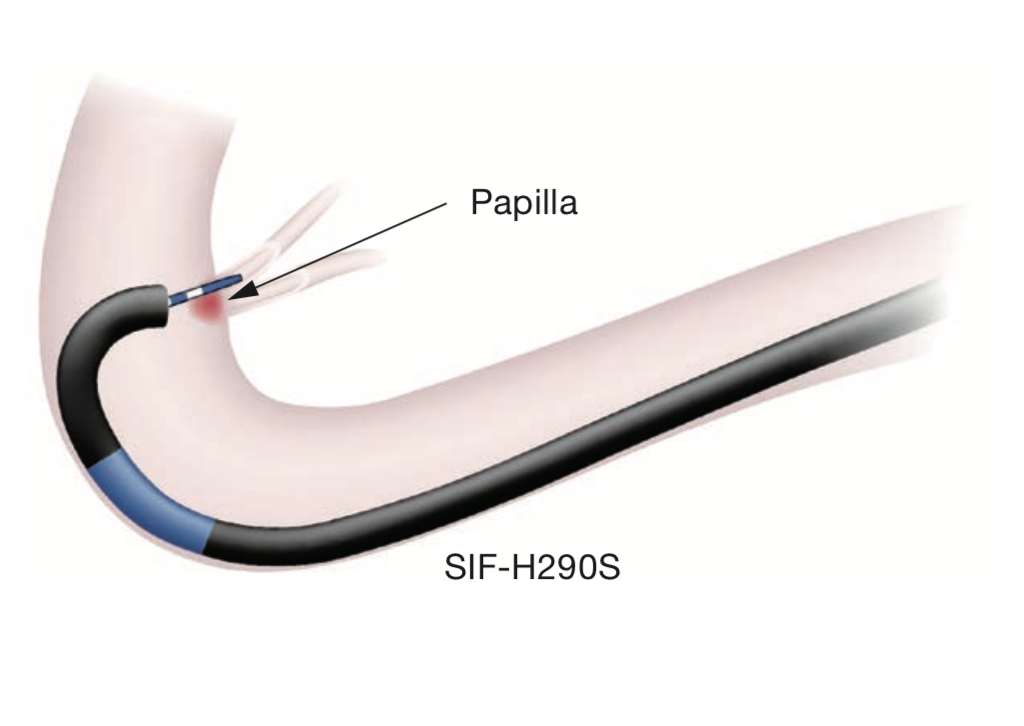
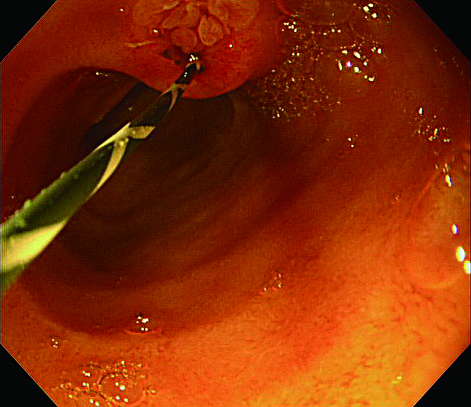
Intubation into bile duct using a forward-viewing endoscope is one of the most difficult techniques to perform. In a non-trivial number of cases, it is only possible to perform cholangiography by using an exquisite combination of a catheter and endoscope. Whatever the case may be conducted with sSBE, it should be kept in mind that catheter enters endoscopic field of view from 7 to 8 o’clock direction (Fig. 5c). Intubation should be performed while aligning papilla and bile duct axis. In cases where you have to insert endoscope blindly, you will have to estimate the alignment.
During intubation, maneuver catheter according to bile duct axis of each papilla (for example, parallel to duodenal wall with a septum type and perpendicular to it with an onion-like type) in the same way as with ordinary ERCP. Generally, we use wire-guided cannulation using VisiGlide2. When and as required, deeper intubation is sometimes performed in combination with trial fluoroscopy. In actual bile duct intubation, manipulation is not limited to catheter manipulation; instead, intubation is often performed in alignment with bile duct axis by adjusting the angulation of the endoscope while minimizing the extruded length of the catheter tip. If fluoroscopy can be performed but the axes of bile duct and catheter cannot be aligned, do not hesitate to use the Radifocus® Guidewire (Terumo). If necessary, a small-diameter catheter (PR-110Q-1, Olympus) or a bendable catheter (SwingTip, PR-233Q, Olympus) can of course also be used. However, the latter model has a large bending radius, making angulation impossible unless part of the catheter tip is extruded from the endoscope tip to a certain degree. Moreover, because the bile duct is positioned in the same direction as the downward angulation direction of the endoscope, it may not be possible to angulate the scope downwards as far as you need to, making this model even less effective in this case.
The biggest advantage of SIF-H290S is that it has an instrument channel diameter of 3.2 mm. This makes it possible to perform a pancreatic duct guidewire technique (or double-guidewire technique) (Fig. 5d), which can be expected to help improve successful bile duct intubation rates. If bile duct intubation is still difficult using the techniques described above, you can try over-the-pancreatic stent pre-cutting after pancreatic stent has been indwelled. If it is difficult even to approach pancreatic duct, you may want to consider free-hand pre-cutting. However, these techniques have a high degree of difficulty and should only be performed by highly experienced endoscopists.
Therapeutic techniques (how to select treatment devices, precautions, etc.)
Thanks to the fact that SIF-H290S incorporates an instrument channel diameter of 3.2 mm and also features a working length of 1,520 mm, almost all currently available treatment devices for bile and pancreatic ducts — including wire-guided devices — can be used. Two of the most commonly performed procedures in clinical cases are choledocholithotomy and biliary stenting, which we will describe below.
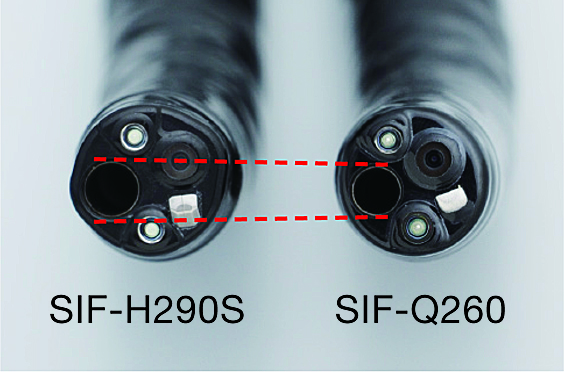
| Model | SIF-H290S | SIF-Q260 |
| Distal end outer diameter | 9.2 mm | 9.2 mm |
| Instrument channel diameter | 3.2 mm | 2.8 mm |
| Working length | 1,520 mm | 2,000 mm |
1) Choledocholithotomy
When you need to remove a stone, it is necessary to treat papilla with endoscopic sphincterotomy (EST), endoscopic papillary balloon dilation (EPBD), or endoscopic papillary large balloon dilation (EPLBD) (Fig. 6a). Since the image of papilla displayed by SIF-H290S’s is upside down, it is difficult to perform safe, secure EST with endoscope maneuvering alone. Thus, EPBD and EPLBD are more commonly performed to treat papilla.
When we perform EPLBD, we try to perform EST whenever possible in order to lower the risk of onset of postprocedural pancreatitis. For EST, we choose a suitable instrument from Olympus’ wire-guided Needle Knife, MTW Endoskopie’s wire-guided push-type or rotatable papillotome for B-II (also usable for R-Y cases).
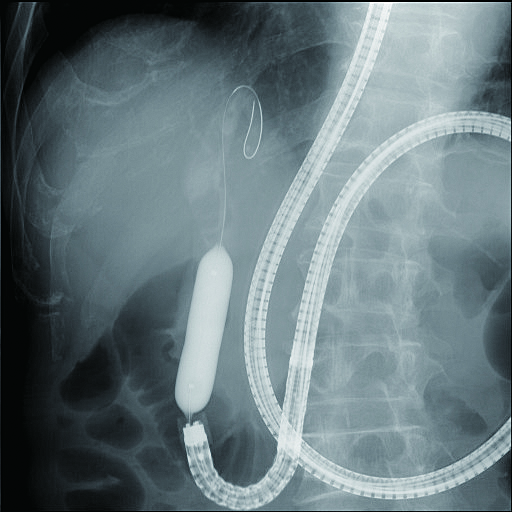
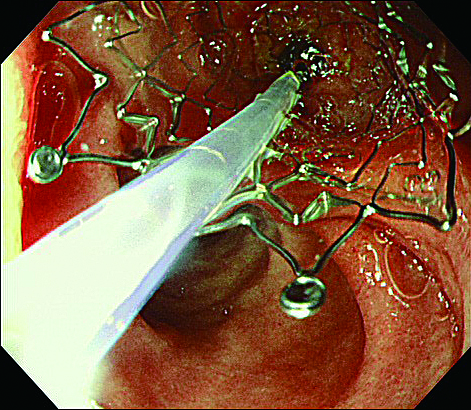
In an actual stone extraction procedure, a wire-guided basket or balloon is inserted into the bile duct via the papilla where EST has been performed. If the stone is large, lithotomy will need to be performed. SIF-H290S’s instrument channel can accommodate a wire-guided mechanical lithotripter (BML-V437QR-30, Olympus) (Figs. 6b, 6c), and this is our first choice.
2) Biliary stenting
Since SIF-H290S incorporates a 3.2-mm diameter channel, a plastic stent as large as 8.5 Fr. can be used. If you are going to use a self-expandable metallic stent (SEMS), you will be able to insert a delivery system as wide as 9 Fr. — which means you can use almost all the uncovered SEMSs and most of the covered SEMSs currently available. However, unlike a duodenoscope, SIF-H290S has a forward-viewing direction of view and is not equipped with a forceps elevator. Hence, it is necessary to use a stent insertion technique that takes advantage of pushing-in of endoscope. For example, by pushing in endoscope while part of SEMS tip is extruded from the endoscope tip, you can easily pass through even a rigid stenosis. As a consequence, this procedure is usually repeated until SEMS is in place (Figs. 7a,7b).

REFERENCES
1) Itoi T, Kasuya K. Surgically altered anatomy and ERCP technique for cholangiopancreatoscopy endoscopist, Roux-en-Y anastomosis. Journal of biliary tract & pancreas 2011;32:987-1007.
2) Itoi T, Ishii K, Sofuni A, et al. Single balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol 2010;105:93-9.
3) Itoi T, Ishii K, Sofuni A, et al. Large balloon dilation following endoscopic sphincterotomy using a balloon-enteroscope for the bile duct stone extractions in patients with Roux-en-Y anastomosis. Dig Liver Dis 2011;43:237-41.
4) Ishii K, Itoi T, Tonozuka R, et al. Balloon enteroscopy-assisted ERCP in patients with Roux-en-Y gastrectomy and intact papilla (with videos). Gastrointest Endosc 2016;83:377-86.
5) Itoi T, Tonozuka R, et al.[Road map to ERCP expert (advanced edition)] ERCP with single balloon enteroscope in patients with surgically altered anatomy, such as Roux-en-Y reconstruction method. Journal of biliary tract & pancreas 2015;36:1271-1274.
- Content Type





