Management of Bile Duct Stones With a Combination Device for Endoscopic Sphincterotomy Plus Endoscopic Papillary Large-Balloon Dilation
Faculty
Todd Baron, MD, FASGE
Professor of Medicine
Director of Advanced Therapeutic Endoscopy
Chapel Hill, North Carolina
Allan P. Weston, MD, FACG
Founder
Digestive Health Center of the Four States
Galena, Kansas
Gastroenterologist
Northwest Arkansas Hospital
Bentonville, Arkansas
James Buxbaum, MD
Associate Professor of Clinical Medicine
University of Southern California, Keck School of Medicine
Director of Endoscopy
Los Angeles County Hospital
Los Angeles, California
Introduction
Endoscopic sphincterotomy (EST) has been used as the primary endoscopic treatment to facilitate removal of bile duct (BD) stones for decades.1 However, use of this modality alone is less successful for removal of multiple and/or large BD stones.2 EST plus endoscopic papillary large-balloon dilation (EST+EPLBD) has emerged as a safe and effective treatment for BD stones. This article discusses the utility of this strategy and reviews the use of StoneMasterV (Olympus Corporation), a unique endoscopic device that combines 2 steps (sphincterotomy and balloon dilation), thereby simplifying stone management by eliminating the need for device exchange.
Management of Difficult Cases of BD Stones
Extraction of ductal stones via endoscopic biliary sphincterotomy followed by retrieval balloon sweep or mechanical lithotripsy with basket can be challenging for the management of some BD stones that lie proximal to a biliary stricture. Size, shape, and number of stones may make extraction difficult. Additionally, it is difficult to remove multiple (≥3), aberrantly shaped, or large (≥12 mm) BD stones after performing EST.2 Investigators have reported high failure rates, and a complication rate in this context, which approaches 13% when using EST alone.3-5 During mechanical lithrotripsy of difficult stones, baskets may also become impacted in the BD requiring higher complexity rescue maneuvers or even surgery.6 Recently, there has been a growing interest in cholangioscope-guided laser or electrohydraulic lithotripsy. However, cholangioscope-guided stone therapy is associated with prolonged procedure time, and contemporary disposable systems are far more expensive than mechanical baskets and other conventional stone removal tools.7,8
In 1982, Staritz and colleagues first described the possible role of biliary dilation to facilitate BD stone removal.9 Wire-guided endoscopic papillary balloon dilation with a small-diameter balloon catheter is easily performed by dilating the intact papilla for 45 to 60 seconds.1 In order to optimize safety and efficacy of this method, Ersoz and colleagues introduced the utility of EST+EPLBD. Dilation with large balloons to increase the diameter of the distal BD opening into the duodenum at the site of sphincterotomy was found to be equally efficacious and potentially safer than extending the already existing sphincterotomy for the management of BD stones.4 Biliary sphincterotomy before papillary balloon dilation directs force away from the pancreas, which protects from postprocedural pancreatitis and expands the biliary orifice, enabling facile and complete stone extraction.10
Current endoscopic society guidelines suggest performing EST+EPLBD for the extraction of selected difficult biliary stones.11,12 This approach is considered to have similar postprocedural pancreatitis rates, but a lower incidence of bleeding and overall complications when compared with EST alone. In a prospective, randomized controlled trial, Stefanidis and colleagues reported that EST+EPLBD was associated with improved rates of BD stone removal (97.7% vs 91.1%) and postprocedural complications (4.4% vs 20.0%) when compared with EST and mechanical lithotripsy for the removal of difficult stones.13 Furthermore, in a systematic analysis of studies, Rouquette and colleagues reported that EST+EPLBD was comparable or superior to other strategies for the management of large common bile duct (CBD) stones. Specifically, the investigators reported that EST+EPLBD was at least as effective as EST.14 EST+EPLBD also reduces the need for additional mechanical lithotripsy and increase in associated technical maneuvers (eg, difficult biliary stones, multiple lithotripsy passes to remove stone fragments, and need for stent placement due to incomplete duct cleareance).15 Adverse event rates (eg, pancreatitis, bleeding, and perforation) were not significantly different when comparing EST+EPLBD with EST. Investigators noted that EST+EPLBD could be performed safely, even in patients with periampullary diverticula and surgically altered anatomy.8
Other studies have suggested that EST+EPLBD is more costeffective than conventional approaches using sphincterotomy followed by retrieval balloon or basket extraction. Itoi and colleagues reported significantly shorter total procedural time (31.6 vs 40.2 minutes) and fluoroscopy time (13.1 vs 21.9 minutes) in the EST+EPLBD group than in the EST group.2 Teoh and colleagues reported a reduction in direct cost of the procedures in the EST+EPLBD and EST (US $5,025 vs US $6,005).16
StoneMasterV for Safe and Effective Combination EST+EPLBD
As reviewed above, EST+EPLBD for the removal of difficult BD stones is safe and effective, and may obviate the need for mechanical lithotripsy or use of a peroral cholangioscope for either electrohydraulic lithotripsy or pulsed-dye laser lithotripsy. However, this approach usually requires 2 devices, a sphincterotomy catheter and a biliary balloon catheter, which require replacing the sphincterome after performing initial sphincterotomy with a balloon device. This exchange prolongs procedural and fluoroscopy times, increases the risk of losing BD access, potentially increases the risk for failed procedures, and increases procedural costs. Further, most large-diameter (ie, >10 mm) dilating balloons have not been specifically designed for use within the biliary tract; their diameters are less than ideal for this indication, sometimes necessitating the serial use of multiple balloons of different diameters or multiple wires of different lengths.It may also be dangerous to use balloons intended for the esophagus or stomach within the narrow working space in the duodenal lumen.
In an effort to solve these limitations by streamlining this process, Olympus America Inc. has developed StoneMasterV— a combination sphincterotome and papillary dilation balloon that merges sphincterotomy and papillary dilation methods to eliminate the need for device exchange (Figure 1).

Figure 1. StoneMasterV combination EST+EPLBD device.
EST+EPLBD, endoscopic sphincterotomy plus endoscopic papillary large-balloon dilation
In addition to combining what has formerly been 2 separate functions into a single device, StoneMasterV has several innovative features to help facilitate the successful removal of BD stones. It is the only short-wire dilation balloon on the market with a C- Channel split for procedural efficiency, and its 4-cm–length balloon provides positional stability and safety. Furthermore, its dilation balloon endoscopic center marker facilitates precise placement, the integrated multisized balloon is continuously adjustable to 3 controlled dilation diameters (12, 15, and 18 mm), and the tapered balloon edges allow the operator to have a clear endoscopic view through the balloon onto the dilated tissue—all of which serve to optimize dilation of the papilla. Additionally, the balloon does not tear when passed back and forth across the elevator.
Other useful features of StoneMasterV include its curved distal end, which orients the cutting wire at a stable 11 o’clock position; this may help reduce efforts in cannulation of the papilla, and ensure optimized incision. Also, the CleverCut coating on the proximal end of the cutting wire minimizes damage to the surrounding tissue, thereby reducing the risk for electrical contact between the wire and the endoscope; this serves to protect the patient and the endoscope. As mentioned, the C-Channel– optimized StoneMasterV supports device exchange for short-wire or traditional over-the-wire techniques.
The lack of the need to exchange from a sphincterotomy device to a balloon dilation device, combined with the advantages of EST+EPLBD, means that StoneMasterV has the potential to reduce procedural time, which may translate into a decrease in anesthesia needs. Also, the ability to remove the entire, intact stone usually obviates the need for mechanical lithotripsy, thereby eliminating the need for additional and often multiple duct sweeping required to clear stone fragments. Complete stone removal prevents the need to place a temporary plastic biliary stent that would require an additional endoscopic procedure for stent and/or stone fragment removal procedure. StoneMasterV is therefore considered to be well suited for management of BD stones, especially larger, barrel- shaped, and multiple stones. Additionally, the StoneMasterV system is only a fraction of the price of contemporary single- use disposable cholangioscopes.
In a single-center retrospective study of patients undergoing removal of BD stones with the use of this combination device, Itoi and colleagues reported complete BD clearance was accomplished in 94% of cases in the first endoscopic session. Also, there were no major intraor postprocedural complications. Based on these data, the investigators concluded that use of this EST+EPLBD combination device is safe and effective to facilitate the removal of large BD stones.17
Conclusion
EST+EPLBD has been demonstrated to be a safe and effective approach to the removal of BD stones that are otherwise difficult to manage via EST alone. StoneMasterV is a unique combination sphincterotome and papillary dilation balloon that merges sphincterotomy and papillary dilation methods into one device to eliminate the need for device exchange, thereby reducing procedural time and simplifying stone management in a cost effective manner. Research indicates that EST+EPLBD reduces the need for mechanical lithotripsy, and potentially the need for cholangioscopy, and their associated procedural costs. These cost and procedural benefits should also translate to the use of StoneMasterV.
References
3. Lauri A, et al. Gut. 1993;34(2):1718-1721.
4. Ersoz G, et al. Gastrointest Endosc. 2003;57(2):156-159.
5. Kim TH, et al. Surg Endosc. 2011;74(5):1127-1132.
6. Thomas M, et al. Am J Gastroenterol. 2007;102(9):1896-1902.
7. Chen YK, et al. Gastrointest Endosc. 2011;74(4):805-814.
8. Kim TH, et al. Surg Endosc. 2011;25(10):3330-3337.
9. Staritz M, et al. Lancet. 1982;1(8284):1306-1307.
11. Chathadi KV, et al. Gastrointest Endosc. 2015;81(4):795-803.
12. Dumonceau JM, et al. Endoscopy. 2010;42(6):503-515.
13. Stefanidis G, et al. Am J Gastroenterol. 2011;106(2):278-285.
14. Rouquette O, et al. World J Gastroenterol. 2014;20(24):7760-7766.
15. Madhoun MF, et al. Diagn Ther Endosc. 2014;2014:309618.
16. Teoh AY, et al. Gastroenterology. 2013;144(2):341-345.e1.
17. Itoi T, et al. Gastrointest Endosc. 2010;72(4):825-830.
Case Study: ERCP in a 67-Year-Old Man for Multiple and Residual CBD Stones
Allan P. Weston, MD, FACG
The patient had a history of smoking 1 pack per day and was recently diagnosed with diabetes mellitus; he presented with painless jaundice and clay-colored stools. He reported no weight loss, itching, or back pain. His physical exam was positive only for marked jaundice without any stigmata of chronic liver disease. Lab results revealed the following levels: total bilirubin, 17.5 mg/dL; aspartate aminotransferase, 90 U/L; alanine aminotransferase, 177 U/L; alkaline phosphatase, 415 mg/dL; and albumin, 3.8 g/dL. Complete blood count and creatinine were normal. A CT scan of the abdomen/pelvis showed dilated intra- and extrahepatic ducts down to the head of the pancreas, a distended gallbladder, but no pancreatic head mass or a dilated pancreatic ductal system.
Endoscopic retrograde cholan gio pancreatography (ERCP) was undertaken with the Olympus America Inc. TJF-Q180V duodenoscope and the Olympus America Inc. CleverCut KD-V431Q-0720 triple-lumen papillotome with 0.025-in VisiGlide guidewire. The ampulla and papilla were normal in appearance. The cholangiogram showed smooth stenosis in the mid-CBD, with multiple stones in the common hepatic duct (CHD) and proximal CBD (Figure 2).
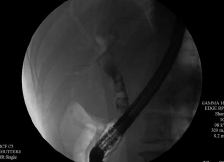
Figure 2. Cholangiogram showing multiple stones in the common hepatic and common bile ducts.
Photo courtesy of Allan P. Weston, MD, FACG.
Biliary sphincterotomy was performed over the guidewire. The CBD stenosis was dilated with a biliary balloon 8 mm wide and 4 cm long and brushed for cytologic samples. The stones above the dilated stenosis were removed with a multisized balloon only partially, with at least 2 residual stones greater than 1 cm in size remaining. Two 10 Fr biliary stents were then placed (10 Fr, 9 cm; 10 Fr, 5 cm).
Liver function tests normalized within 2 weeks, and an upper endoscopic ultrasonographic examination of the pancreas/biliary tree was conducted with the Olympus America Inc. GF-UE160-AL5 radial array echoendoscope. Neither a pancreatic head nor an ampullary mass was noted, nor was chronic pancreatitis. Multiple gallstones were seen (largest, 1.5 cm). Two residual CHD stones were noted (1 and 1.2 cm) along with intact CBD, 2 stents, and mild symmetric thickening of the CBD wall.
He underwent laparoscopic gallbladder resection and then returned for a second ERCP procedure; the goal was to remove any residual CHD/CBD stones with the Olympus America Inc. StoneMasterV. After the second ERCP procedure, both CBD stents were removed with a snare. The StoneMasterV was used to cannulate the CBD and CBD stenosis, and the sphincterotomy incision was dilated to 12 mm. The residual stones were then captured and removed with a 4-wire stone retrieval basket over a guidewire. Finally, a multisized balloon catheter was used to sweep the CHD and CBD multiple times, revealing complete clearance of the biliary tree of residual stones.
Use of StoneMasterV device markedly shortened the procedural time required to remove the residual stones after the second ERCP procedure by both dilating the biliary sphincter as well as the benign stenosis of the mid-/distal CBD, allowing for the retained stones to be removed without resorting to mechanical lithotripsy or cholangioscopy and a laser lithotripsy device. Using the StoneMasterV in the initial ERCP procedure may have eliminated the need for a second procedure by achieving complete ductal clearance.
- Content Type





