Suggested Indications for Colorectal ESD
Among lesions that require en-bloc endoscopic resection,
the following are considered to be indications for colorectal ESD.
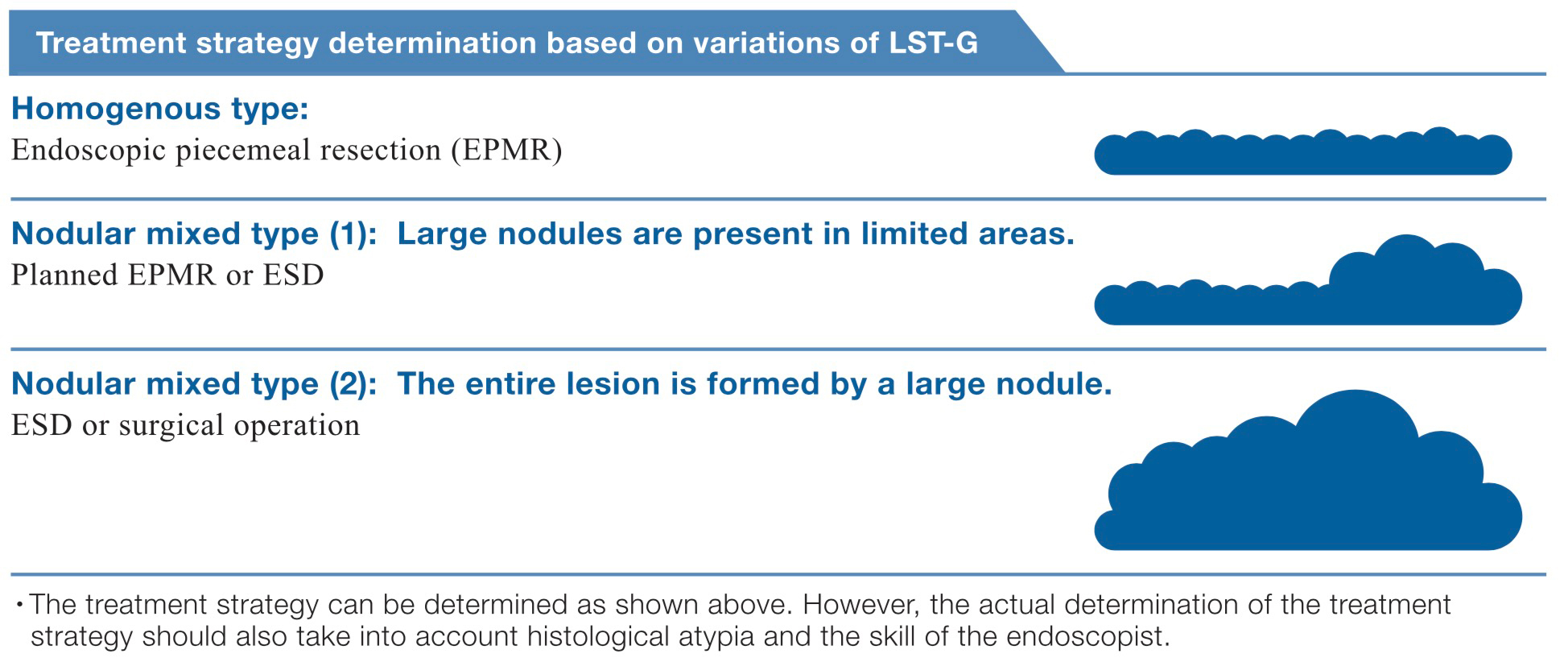
1.Lesions that are hard to resect en bloc using a snare:
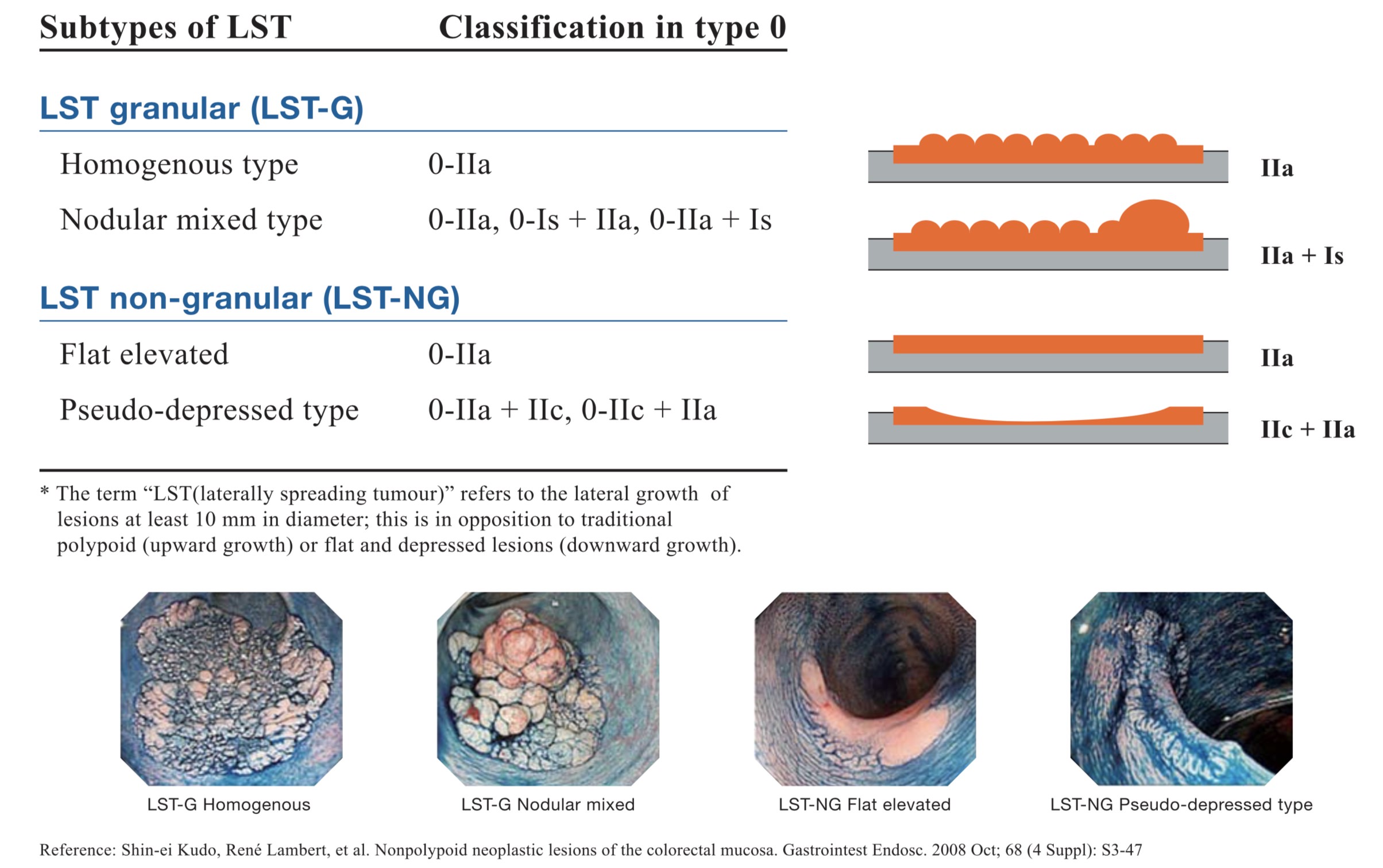
・Laterally spreading tumours of the non-granular type (LST-NG), particularly the pseudo-depressed type.
・Lesions presenting Type V1 pit pattern.
・SM carcinomas with scanty invasion.
・Large depressed type tumours.
・Large elevated lesions suspected to be carcinoma .
2.Intramucosal lesions accompanied by submucosal fibrosis .
3.Sporadic local tumours located at chronic inflammations such as ulcerative colitis .
4.Local residual early carcinoma after endoscopic resection .
Notes)
*1. Includes tall laterally spreading tumours of granular type (LST-G).
*2. Lesions caused by prolapse due to biopsy or lesion peristalsis.
*3. Technical difficulty is high.
Supplement
1.Both magnifying observation results as well as ordinary endoscopic observation should be used to determine whether or not colorectal ESD is indicated.
2.In principle, SM carcinomas should be eliminated from the indication when invasion is clearly massive.
3.With laterally spreading tumours of the granular type (LST-G), the treatment strategy should be based on the visually observed characteristics and the pit pattern diagnosis with magnifying observation as shown below. The large nodular area and Type V pit pattern area should not be divided.
4. A small SMT (submucosal tumours ) localised in the submucosa can also be a target for indication
Degree of Difficulty of Colorectal ESD by Region
| Region | Colorectal ESD Precautions According to Organ Characteristics |
| Rectum | Retroflexion is required. Special care is required in the rectum because it contains many more blood vessels than the colon. Careless retroflexion of the scope may pose a risk of perforation, so please pay attention when manoeuvring the scope. |
| Sigmoidcolon | In this region, the scope tends to cause paradoxical movement, thereby making treatment difficult. As the lumen is narrow and bent, it is important to secure the field of view.(Advanced training required.) |
| Descending colon | Restricted scope manoeuvrability sometimes makes the procedure difficult. Please pay special attention to the area around the splenic flexure due to respiratory movement. Transverse colon- The scope tends to cause paradoxical movement in certain areas. It is difficult to secure the field of view at the splenic flexure, middle transverse colon and hepatic flexure. (Advance training required.) |
| Ascending colon | In spite of respiratory movement, the lumen is relatively wide so it is easy to secure the field of view except in the area around the hepatic flexure. However, an extended procedure tends to cause deflection of the sigmoid colon. |
| Cecum | ESD is difficult because the wall is thin and the knife has to be applied perpendicularly to the thin wall. |
Subtypes of LST* lesions: Morphologic classification of LST lesions and their correspondence in the Paris-Japanese classification
Notes on Colorectal ESD for First-Time Practitionars
The main reason for the technical difficulty of colorectal ESD is the difficulty of manoeuvring the endoscope with respect to the lesion. The anatomical characteristics of the colon and rectum (thin wall and the presence of peristalsis, folds, bends, fecal fluid, etc.) also add to the difficulty.
Perforation of the colon wall is a serious concern as there is a high likelihood of concurrent peritonitis due to fecal fluid leakage which may require surgery. Perforation of the stomach wall, on the other hand, can usually be treated successfully with conservative management.
The degree of difficulty of colorectal ESD is determined more by the manoeuvrability of the scope than by the size or shape of the lesion. Conducting the procedure in the same way as gastric ESD could produce a perforation. Before performing ESD for the first time, it is important to be acquainted with the particularities of the colon and rectum.
If the insertion technique based on total freedom of scope control has not been mastered, colorectal ESD should not be attempted. It is recommended that gastric ESD be tried first, and then an actual colorectal ESD be observed to understand how it differs from gastric ESD. Initially, colorectal ESD should be performed under the supervision of an expert endoscopist on a lesion with a low degree of difficulty specifically, a relatively small rectal lesion in an area where scope control is relatively easy.
Please note that it is important to design an effective strategy before proceeding with colorectal ESD,
including how and when to reposition the patient.
[Recommended steps for mastering colorectal ESD techniques]
[STEP1]
Master the handling of the scope, ancillary equipment, endotherapy devices and medications.
[STEP2]
Practice the scope manoeuvring technique until you can perform an upper gastrointestinal examination
without difficulty.
[STEP3]
Master the colonoscopy insertion technique and the diagnostics.
[STEP4]
Learn the upper gastrointestinal and colorectal treatment techniques including the haemostasis technique,polypectomy, EMR and EPMR. 〇nce you have successfully completed Steps 1 to 4, you are ready to safelyperform a basic ESD procedure.
You can then proceed to the following steps.
[STEP5]
Enhance your knowledge and technique by observing or assisting in actual ESD procedures, as well as by
part1c1pating in simulations and various live demonstrations using animal models.
[STEP6]
Begin ESD by d” 1ssectmg a lesion in the gastric antrum under the guidance of an expert endoscopist. Then
master ESD of safe gastric lesions and the method of treatment of accidental symptoms. After completing these
steps, you will be ready to perform oesophageal ESD and colorectal ESD with the highest degree of difficulty.
Flow of colorectal ESD techniques

Thorough preparation is required before starting ESD.
Marking is basically not required, as the extent of colorectal lesion can be distinguished easily.
To ensure an efficient procedure, plan how to proceed with the incision and dissection beforehand.
Apply local injection only to the area where you are about to incise. This will maintain the lifting effect of the mucosa.
Incise the mucosa and then dissect the submucosa below it for a certain degree.
Repeat the mucosa! incision and submucosal dissection alternately until the whole lesion is dissected.
→To extend the submucosa and ensure a smoother procedure, use local injections and adjust the patient's position as necessary.
→Frequent haemostasis is required to maintain a clear view.Observe the ulcer floor after treatment and treat the vessels with the potentials of delayed bleeding with haemostatic forceps.
- Content Type