DISCLAIMER
The surgical technique herein is presented to demonstrate the method utilized by S. Van Slycke, MD, of the Department of General and Endocrine Surgery at the OLV Clinic, Aalst, Belgium. The information on the products and procedures contained in this brochure does not represent and does not constitute medical advice or recommendations and should not be relied upon as such.
This information does not purport to constitute any diagnostic or therapeutic statement with regard to any individual medical case. Each patient must be examined and advised individually, and this brochure does not replace the need for such examination and/or advice in whole or in part.
This brochure should not be considered as a substitute for carefully reading all applicable labeling, including the instructions for use (IFU) supplied with the devices. Before using any product, please thoroughly review the relevant user manual(s) for instructions, including, but not limited to, contraindications, warnings, precautions, and adverse effects. Please note: It is the clinicians’ responsibility to decide which instrument mode and settings they use in each clinical situation.
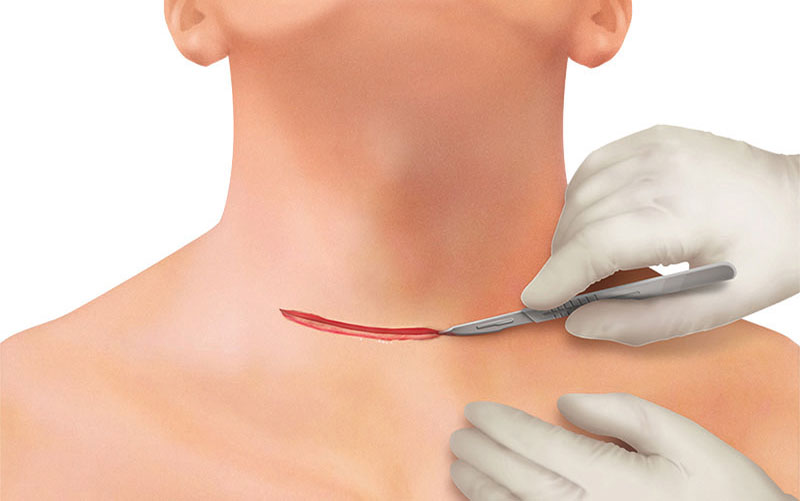
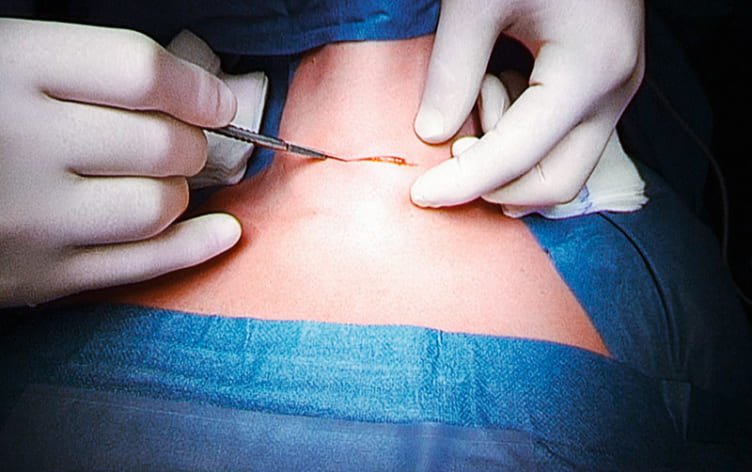
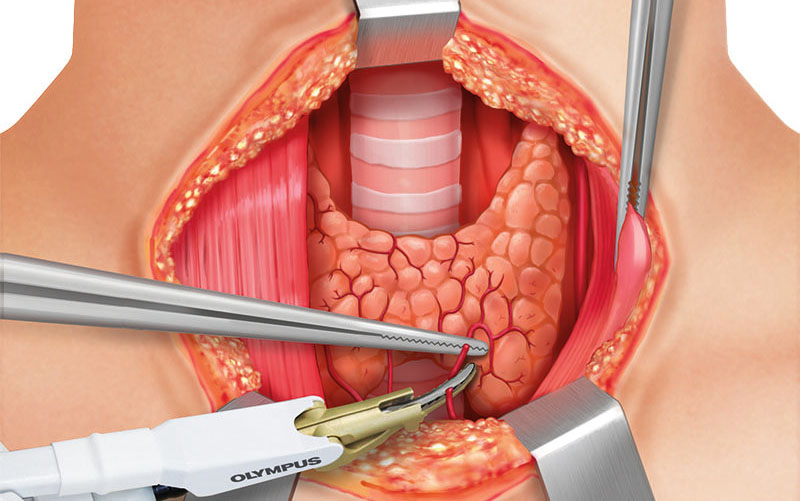
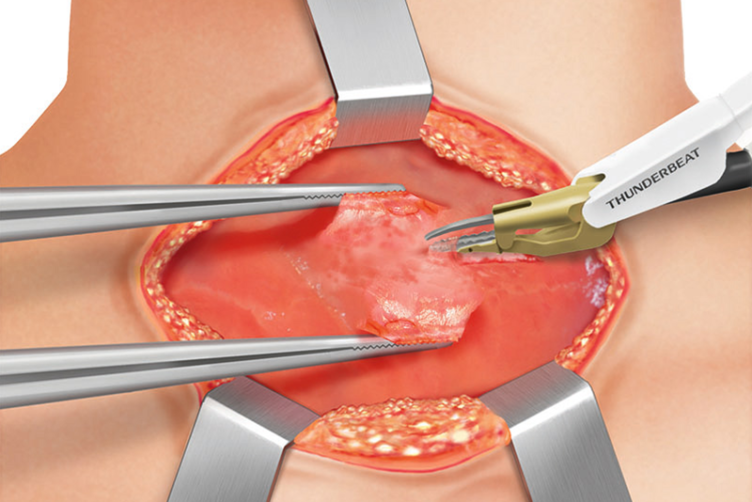
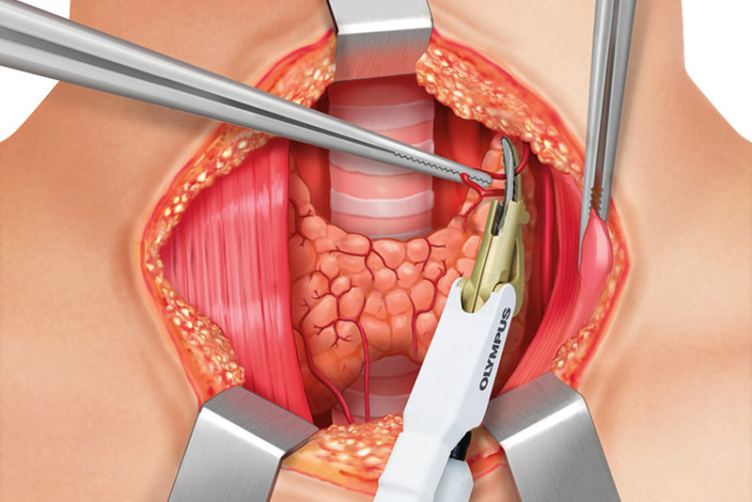
ACCESS TO THE THYROID GLAND
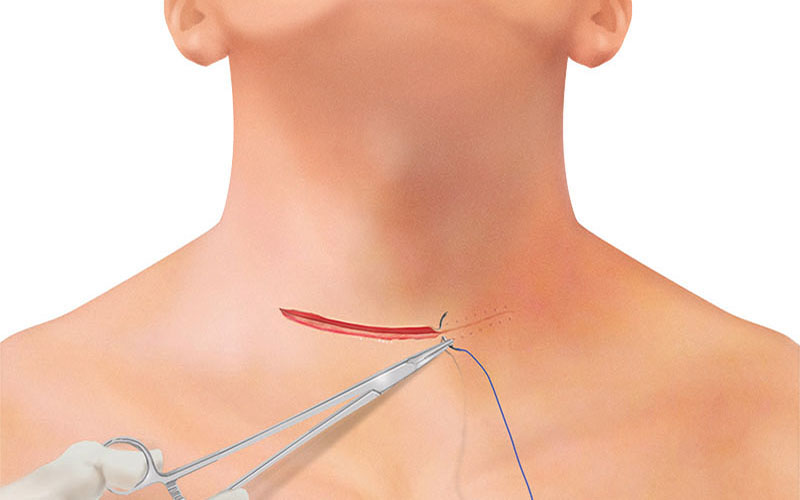
Two fingers above the sternoclavicular joint, a 4–8 cm collar skin incision is made with a scalpel. Further dissection and cutting through subcutaneous fat is continued with THUNDERBEAT or a monopolar pencil (and bipolar forceps for hemostasis).
The fibers of the platysma muscle are dissected from underlying cervical fascia and incised horizontally with THUNDERBEAT and then retracted. Hemostasis can be provided via THUNDERBEAT SEAL mode or a monopolar pencil and/or bipolar forceps.
ACCESS TO THE THYROID GLAND
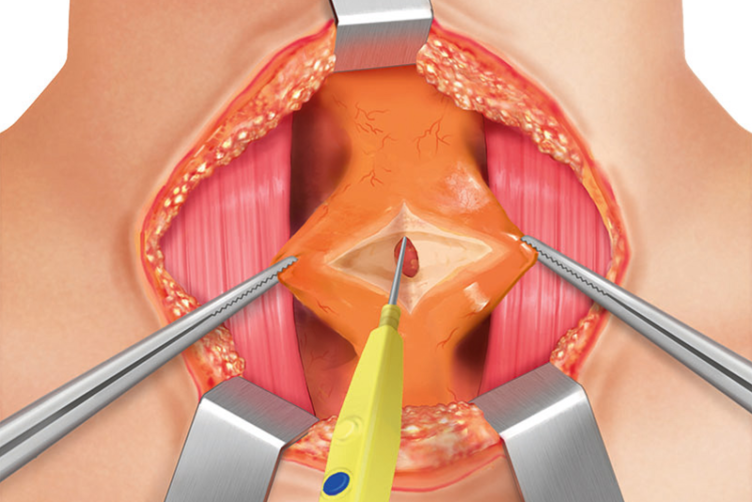
Upward and downward skin flaps are created with respect to the anterior jugular veins, which can easily be harmed (in this case, one can divide them with ligatures or use the THUNDERBEAT). The downward skin flap is created toward the suprasternal notch.
Underneath the platysma muscles, the strap muscles (infrahyoid muscles as a group of four pairs) can be found.
The four infrahyoid muscle pairs are the sternohyoid, sternothyroid, thyrohyoid, and omohyoid muscles.
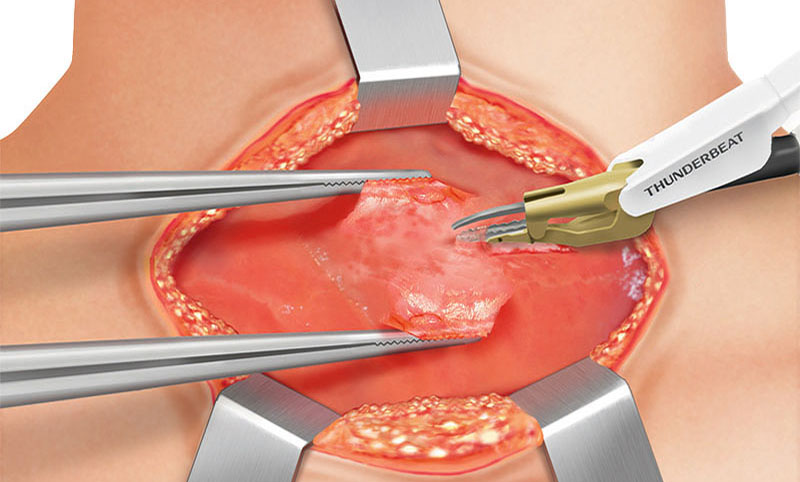
These are dissected bluntly and sharply in a vertical way by division of the avascular midline plane from the thyroid cartilage toward the suprasternal notch using monopolar cauterization or using THUNDERBEAT.
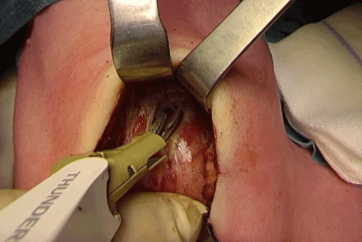
The medial cervical fascia is incised and a plane between the strap muscles and the thyroid gland is created with THUNDERBEAT or a bipolar device. Bleeding of the strap muscles can be controlled by using THUNDERBEAT SEAL mode. The strap muscles are separated from the underlying thyroid capsule and retracted laterally.
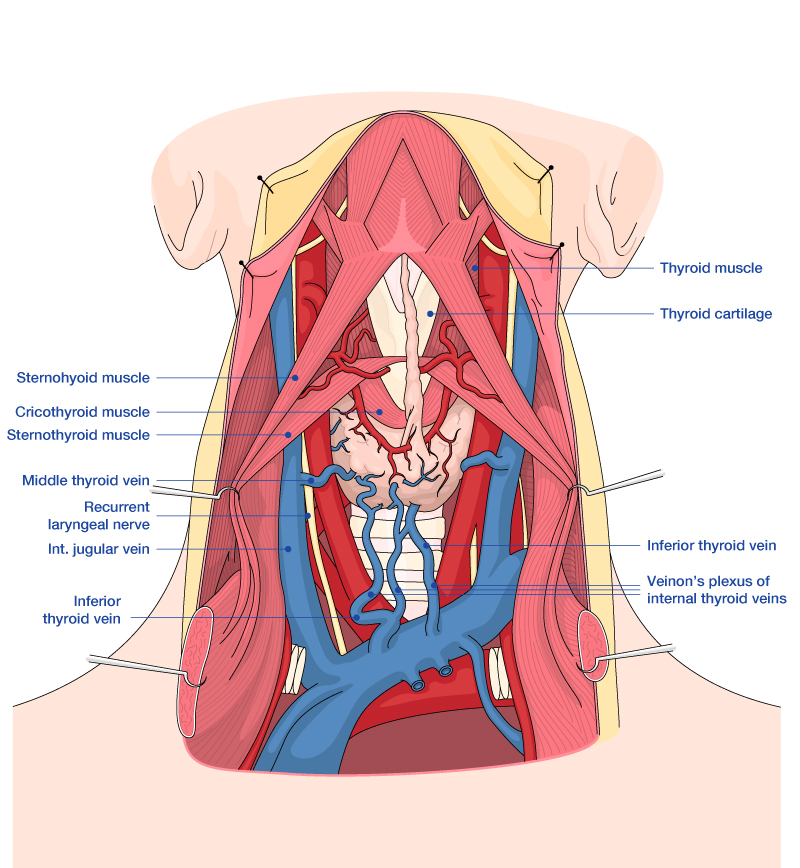
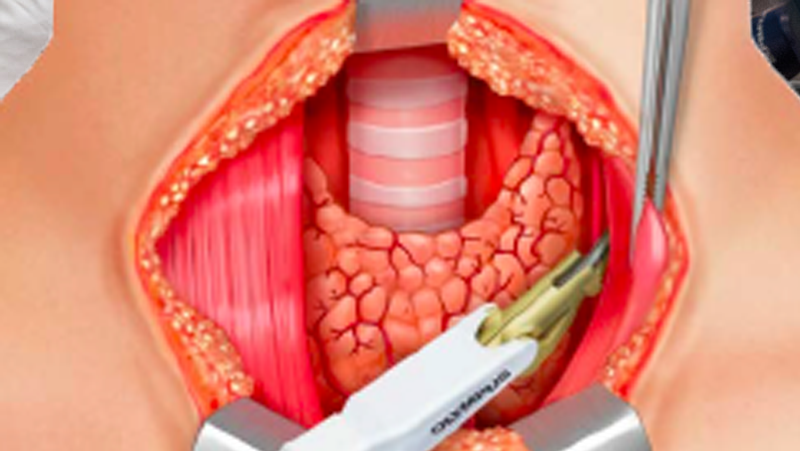
LEFT LATERAL THYROID DISSECTION
The dissection is continued laterally toward the jugular carotid sheath, where the common carotid artery, vagus nerve, and internal jugular vein are found. The lateral mobilization of the lobe should be done as far away from the gland as possible.
FURTHER LEFT LATERAL DISSECTION
The sheath is opened by cold dissection using a mosquito clamp or THUNDERBEAT, and the vagus nerve is dissected under constant neuromonitoring. The internal jugular vein can be divided by THUNDERBEAT. With medial traction of the lobe, the middle thyroid vein and branches of inferior thyroid artery can be seen. They can be ligated with THUNDERBEAT. Now, after opening the carotid sheath, the V1 signal is acquired (vagus stimulation).
For safe dissection, the vocal nerves should be monitored constantly during the whole procedure.
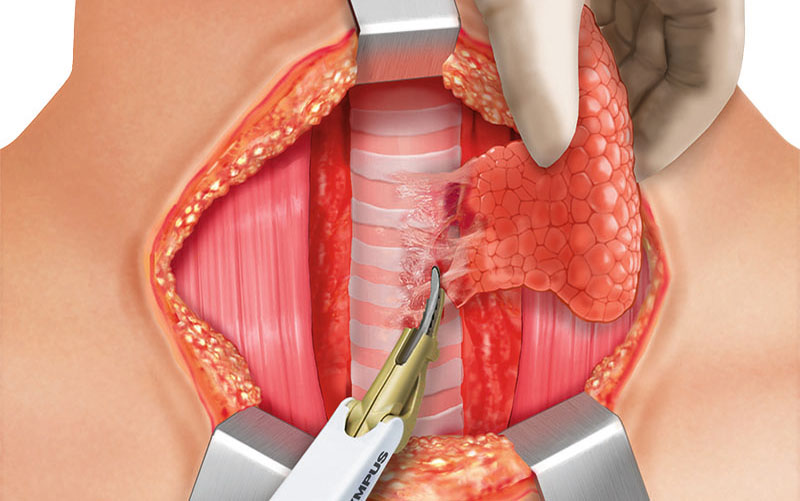
MEDIAL AND LEFT SUPERIOR THYROID GLAND DISSECTION
After the lateral dissection is finished, the procedure continues with the medial part of the thyroid and the pyramidal lobe. The pyramidal lobe is the extension of the isthmus on the midline, going to the base of the tongue; on either side just above the cricothyroid muscle, the supporting blood vessels are divided by THUNDERBEAT.
Damage to the cricothyroid muscles and external branch of the superior laryngeal nerve that run parallel has to be avoided.
If present, the pyramidal lobe is dissected first; ligation of its blood vessels using THUNDERBEAT.
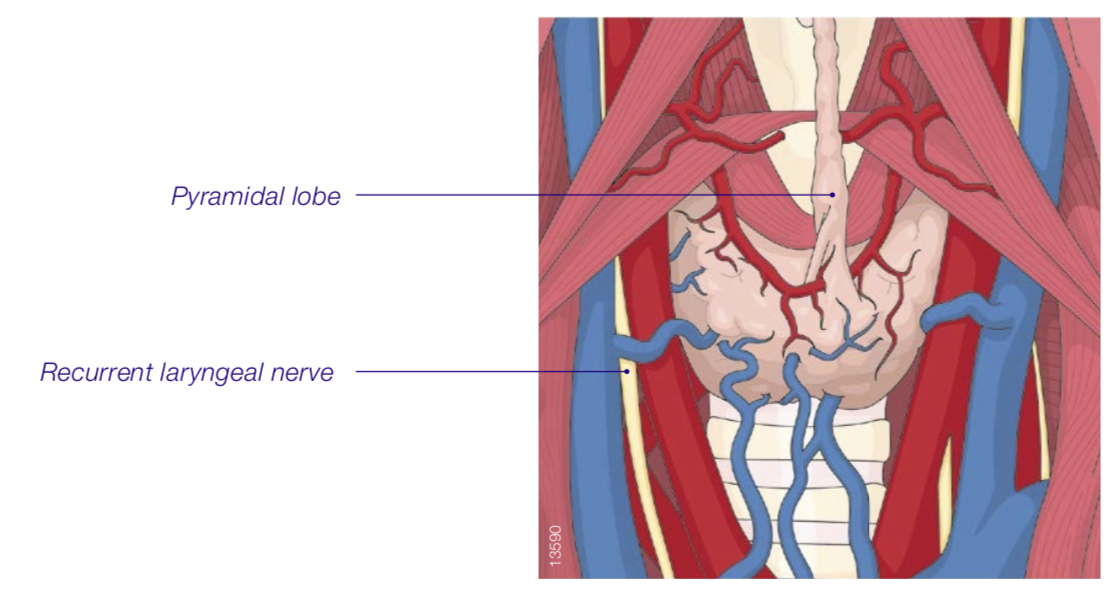
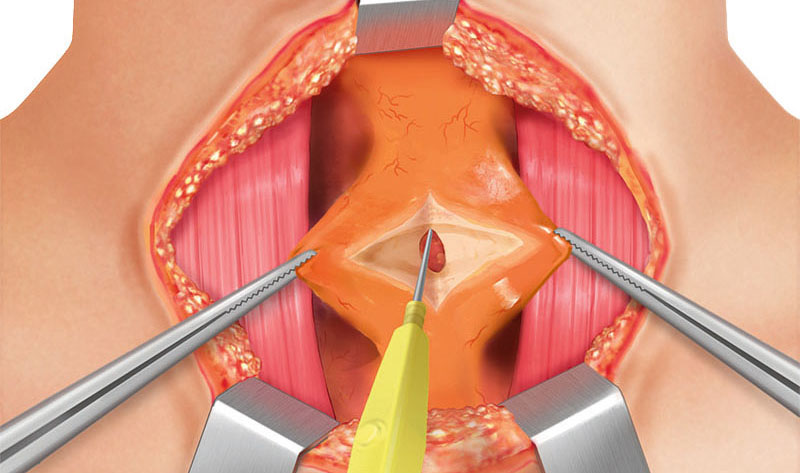
The medial dissection at the isthmus is continued at the level of the cricothyroid muscle using Kelly or mosquito clamps or with nonactivated THUNDERBEAT in order to find a plane between the thyroid lobe and the cricothyroid muscle itself. The dissection continues toward the superior pole of the lobe.
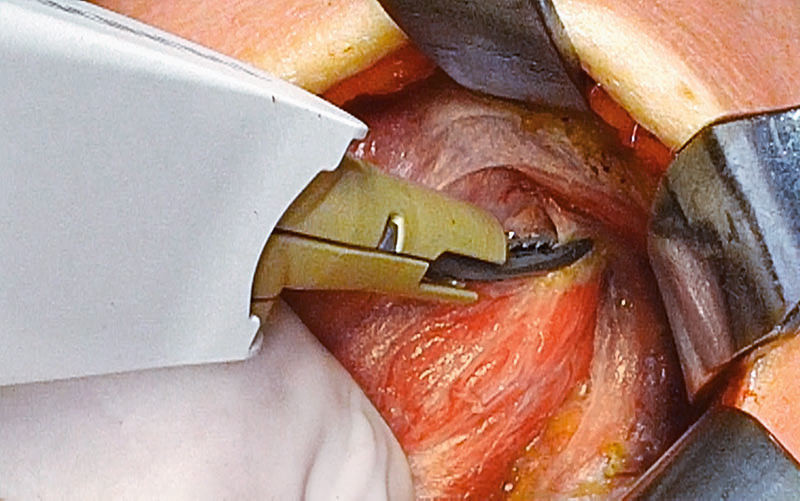
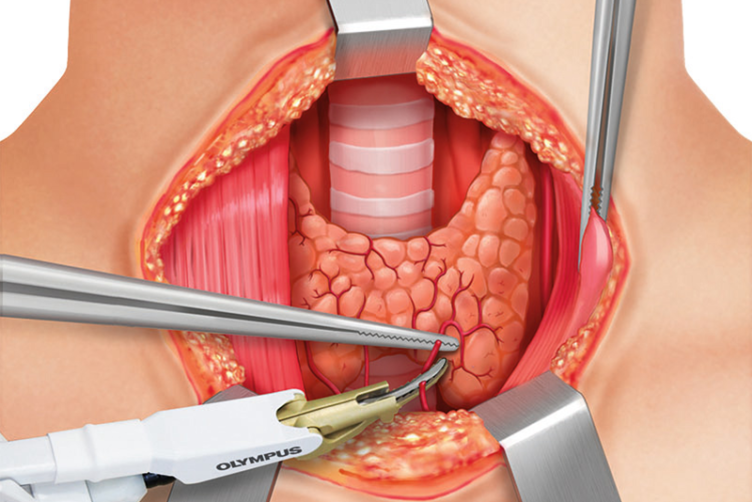
DISSECTION OF LEFT SUPERIOR THYROID POLE
The dissection continues at the superior thyroid pole, including ligation of the superior thyroid artery and its branches with small bites made using THUNDERBEAT.
The superior laryngeal nerve needs to be identified and monitored as it is located close to the superior thyroid artery.
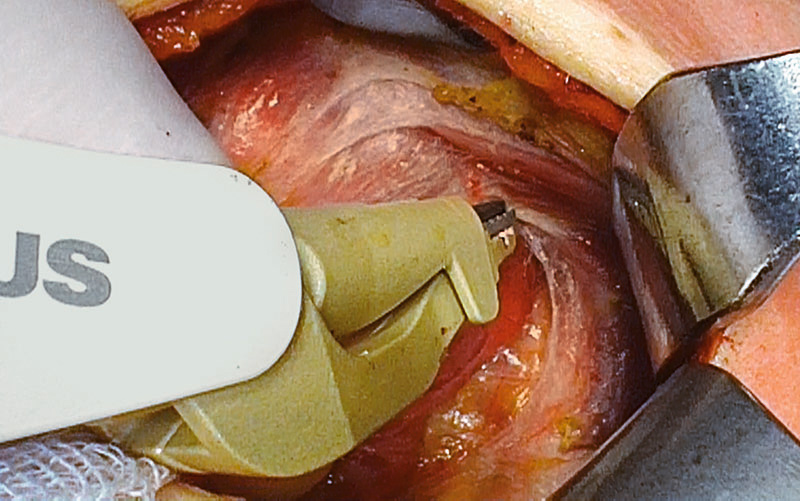
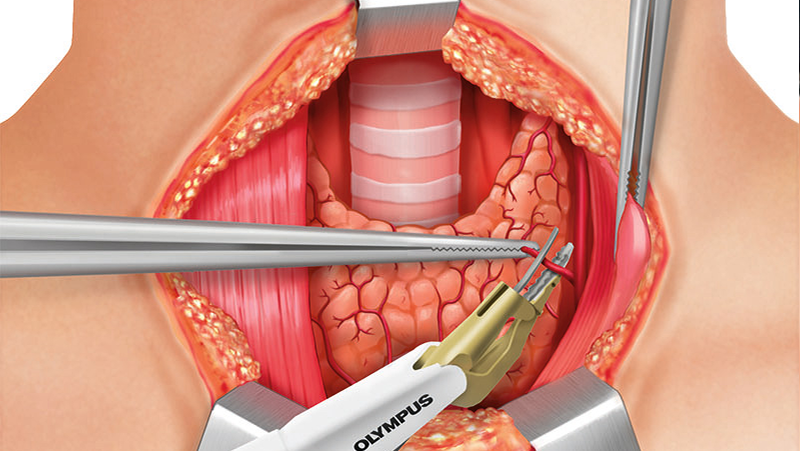
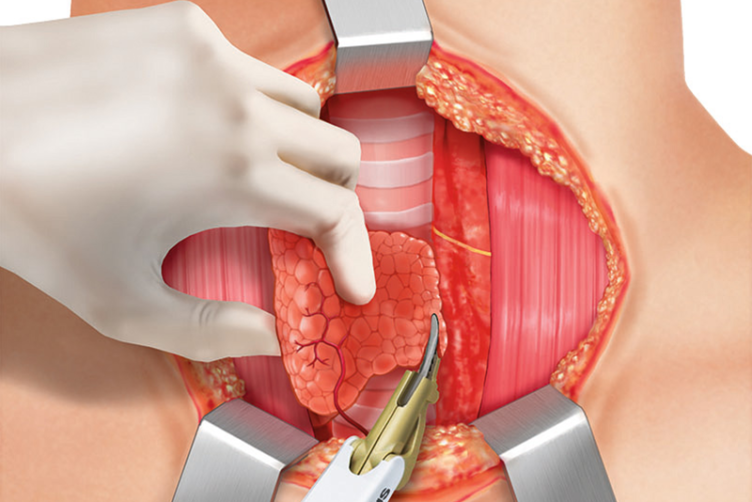
POSTERIOR DISSECTION OF LEFT THYROID LOBE
Posterior to the left thyroid lobe, distal branches of the superior thyroid vessels are sealed and divided close to the thyroid capsule. The recurrent laryngeal nerve has to be identified and monitored.
FURTHER POSTERIOR DISSECTION OF LEFT THYROID LOBE
The posterior mobilization continues along the course of the recurrent laryngeal nerve with constant neuromonitoring and documentation. The left superior parathyroid glands posterior to the left thyroid lobe are identified. They are carefully separated from the thyroid capsule together with their vascular pedicles.
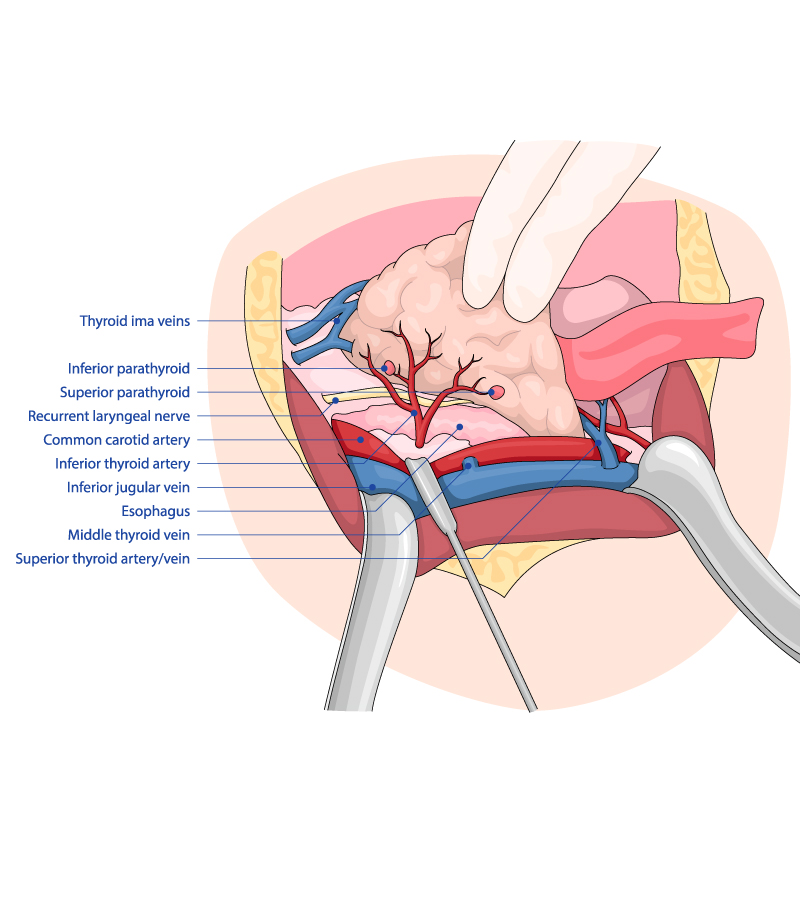
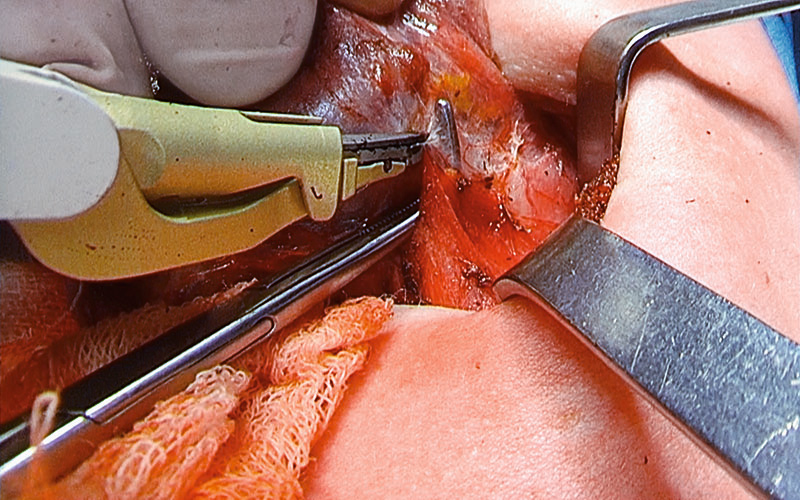
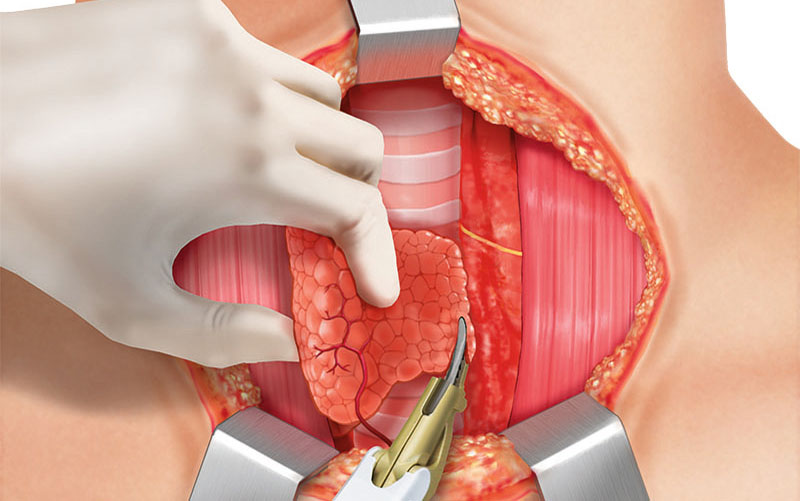
DISSECTION OF LEFT INFERIOR THYROID LOBE
Now the dissection of the lower pole is started in front of the trachea. The inferior thyroid vessels (branches of the inferior thyroid arteries and veins) are identified and ligated using THUNDERBEAT without any traction.
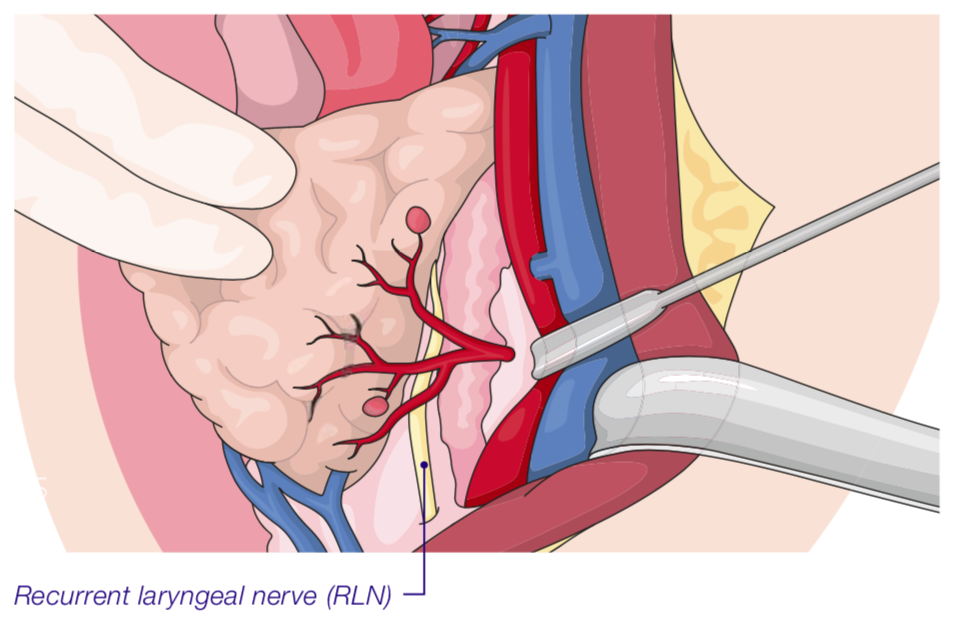
The lower pole has to be completely mobilized by continuing the dissection paratracheally where the recurrent laryngeal nerve (RLN) runs, crossing the inferior thyroid vessels and their branches. The RLN needs to be checked and the R1 signal must be documented.
The inferior parathyroid glands have to be identified and separated away from the posterior thyroid capsule by leaving the respective vessels intact.
PARATRACHEAL DISSECTION OF THE THYROID
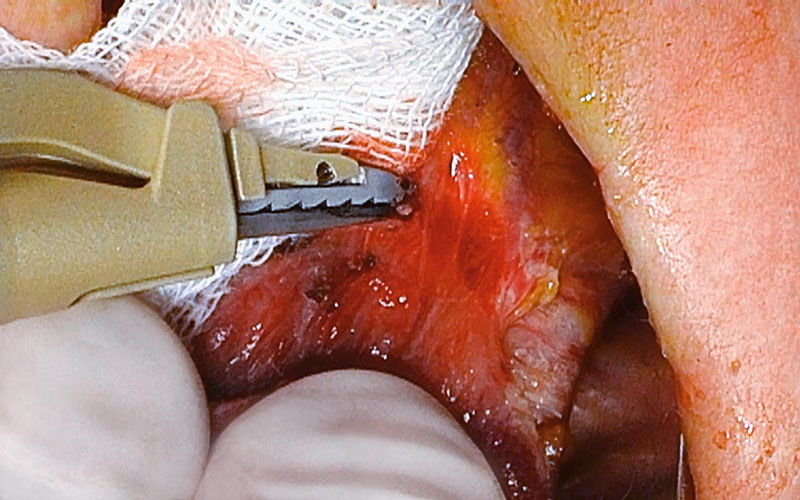
Very careful dissection between the thyroid lobe and the RLN, from inferior to superior, parallel to the course of the RLN is performed.
A possible accessory ima thyroid artery, running from caudally toward the inferior pole needs to be seen and monitored. A critical area is the ligament of Berry with its fine, strong tissue (attachment of thyroid to trachea) where very careful dissection is needed because branches of the superior thyroid artery may run behind the nerve and need to be ligated carefully.
Too much traction has to be avoided. Thermal effects and residual heat of any energy device could be dangerous here.
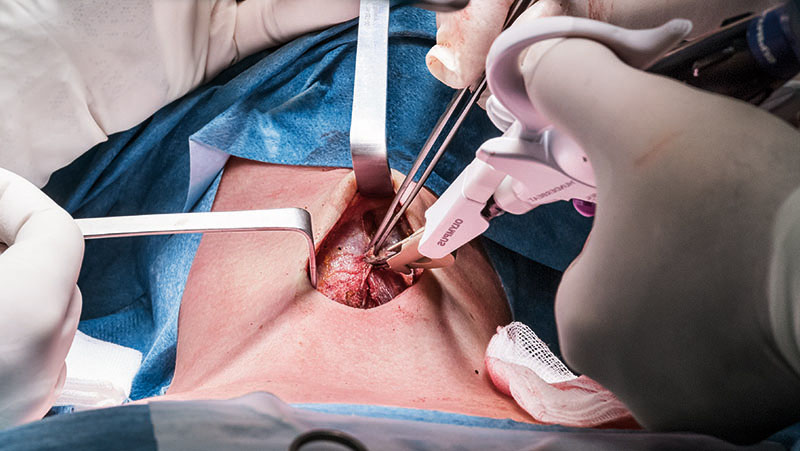
COMPLETION OF LOBECTOMY
The transection of the isthmus is completed. The pretracheal adhesions are divided using THUNDERBEAT, and a complete hemithyroidectomy is performed. The RLN and the vagus nerve are finally monitored and the R2 and V2 signals are documented. Complete hemostasis has to be secured prior to closure. Placing the patient in a head-down position with the anaesthesiologist, the Valsalva maneuver is performed on the patient to check for bleeding. Lymph node dissection is performed if necessary.
FURTHER STEPS
In the Case of a Partial Thyroidectomy
Placement of a drain and wound closure.
In the Case of a Total Thyroidectomy
Repetition of steps for thyroid lobe on opposite site, placement of a drain, and wound closure.
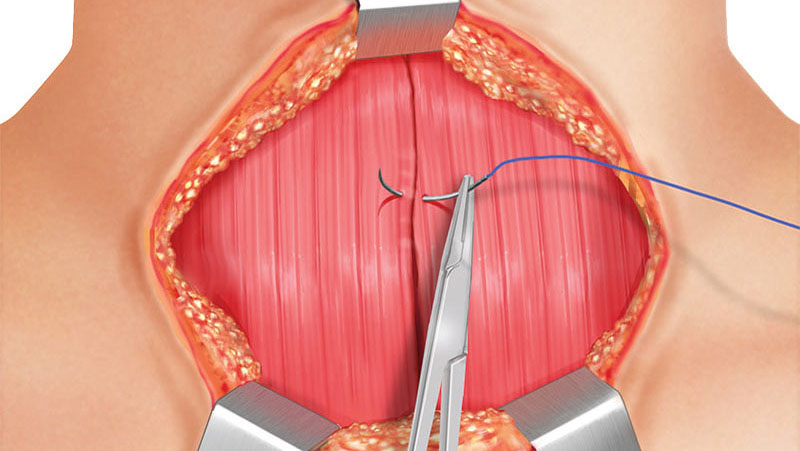
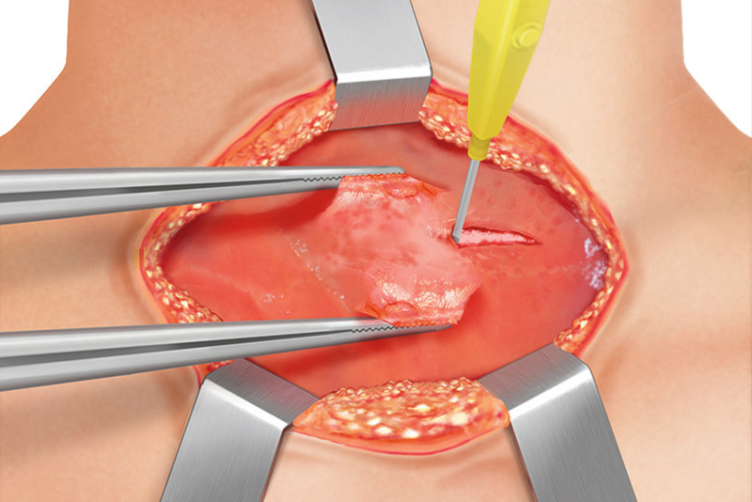
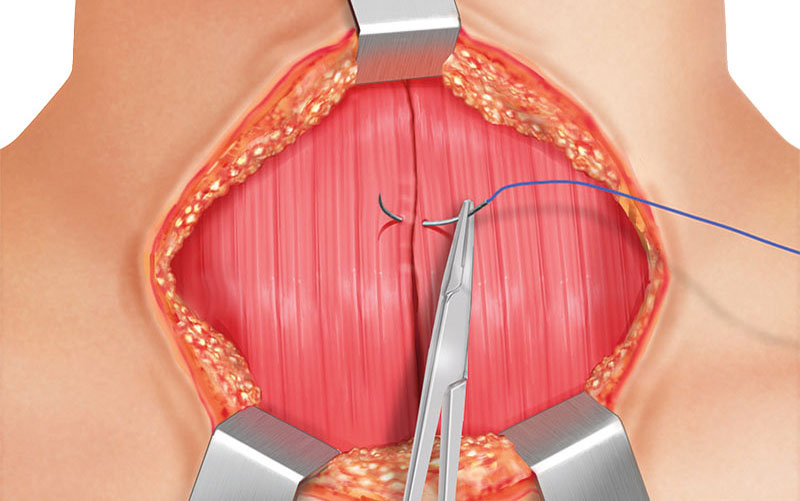
CLOSING MUSCLE LAYERS
The strap muscles are closed at the midline with continuous running suture with resorbable 4-0 suture material. The platysma fibers have to be sutured with interrupted stitches using resorbable 4-0 suture material.
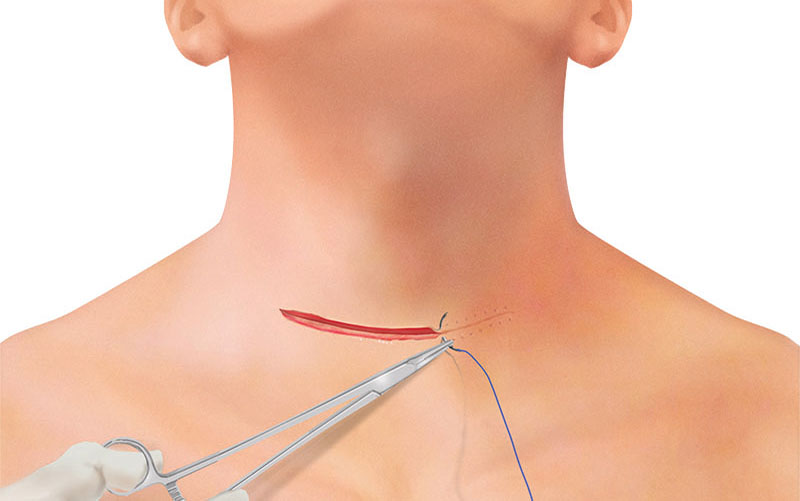
WOUND CLOSURE (INTRACUTANEOUS SUTURING)
The skin itself is closed with a continuous suture and resorbable 4-0 suture material. If applicable, steristrips or skin glue is used.
SUMMARY




- Content Type