Paweł Rogalski
MD, PhD
Introduction
Colonoscopy with polypectomy is the cornerstone of colorectal cancer (CRC) prevention. Its use within screening programmes allows for a significant reduction in the morbidity and mortality due to CRC. A prerequisite for the effectiveness of such programmes is high quality of endoscopic procedures. Improvement in the quality of colonoscopy is currently executed through two strategies: (1) improving imaging techniques to increase the detection of adenomas, (2) modifying colorectal lesion removal techniques to reduce the rate of incomplete resections while keeping the risk of complications as low as possible.
Endoscopic removal of colorectal lesions by snare
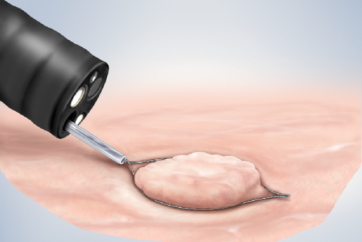
The choice of the appropriate endoscopic resection method should take into account: the size, morphology, location and most likely histological type of the lesion. In recent years, snare polypectomy without electrocoagulation („cold”) has become the standard treatment for small (<10 mm) colorectal polyps. This technique ensures a high rate of complete resections and provides good quality histological material. It is also simple and safe. The efficacy of this method can be further increased using dedicated cold polypectomy snares made of thin (0.3 mm) braided wire, facilitating the removal of lesions with a margin of healthy tissue.
Due to the extent of laterally spreading tumours (LST), en-bloc resection of these lesions with polypectomy snare is often not possible. Nevertheless, most colorectal lesions do not show submucosal invasion and can be successfully resected with piecemeal mucosectomy technique (piecemeal EMR). The key to success in this type of endoscopic resection is the correct qualification of the patient for the procedure. Piecemeal EMR can be used to remove serrated lesions or classic adenomas with a homogeneous, granular surface (LST-G-H).
If the risk of submucosal invasion is high, the aim should be to remove the lesion en-bloc, e.g. by endoscopic submucosal dissection (ESD) or endoscopic full-thickness resection (EFTR). This applies especially to pseudodepressed lesions (LST-NG-PD) or LSTs with a non-granular morphology (LST-NG) or lesions with an irregular surface pattern.
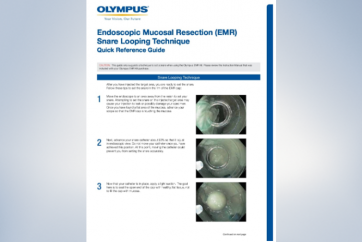
Additional techniques increasing the efficacy and safety of endoscopic resections
Recent literature reports demonstrate the benefits of additional techniques and modifications to classical endoscopic resections performed with polypectomy snares. Currently, adjuvant thermal ablation of margins at the EMR site is recommended to reduce the recurrence rate of adenomas. On the other hand, prophylactic clip closure of mucosal defects >20 mm in the right side of the colon significantly reduces the frequency of delayed bleeding. Potential benefits have also been demonstrated in terms of increased en-bloc resection rates in underwater EMR and reduced rates of delayed bleeding and delayed perforation in cold EMR.
SnareMaster Plus
The Olympus SnareMaster Plus is a hybrid snare that combines the advantages of a dedicated snare for simple cold or hot polypectomy as well as a snare for EMR. The tool is available in two sizes, 10 mm and 15 mm, allowing for comfortable polypectomy of lesions less than 10 mm in size as well as endoscopic resection of large LSTs respectively. At the same time, the smooth adjustment of the snare opening allows the size of the snare to be adapted to the clinical situation. The thin wire, combined with optimum stiffness, allows the safe grasping and clean cutting of large lesion fragments with a safe margin of healthy tissue, without traumatization of the tissue around the resection site. The hexagonal shape further increases the stiffness of the snare and helps to maintain the correct cutting plane, which is particularly beneficial in lesions with significant fibrosis in the submucosal layer. The snare can be successfully used to remove lesions using the classic EMR technique with electrocoagulation, as well as cold EMR or underwater procedures.
The principles I follow for the endoscopic removal of colorectal lesions by snare
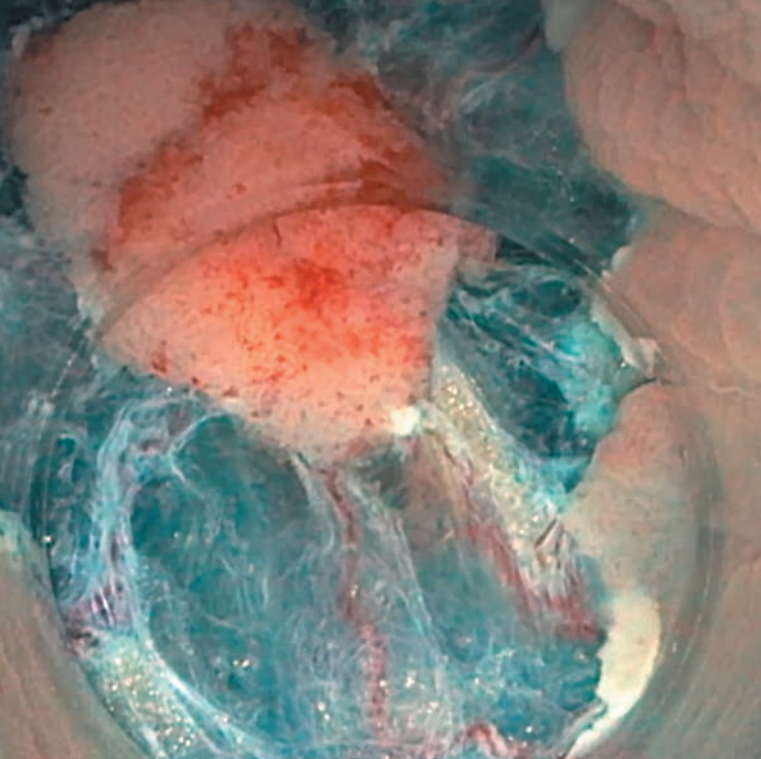
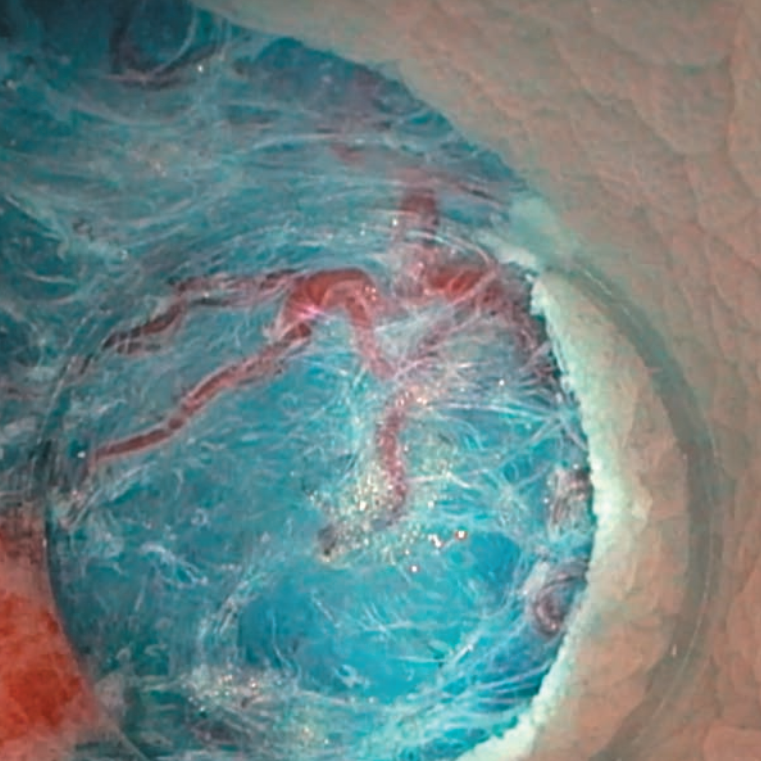
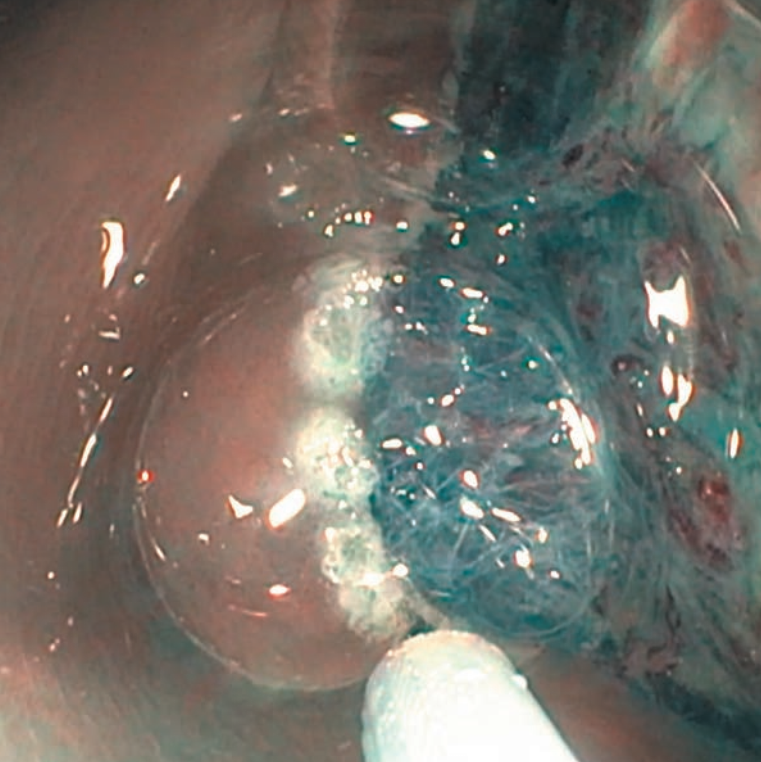
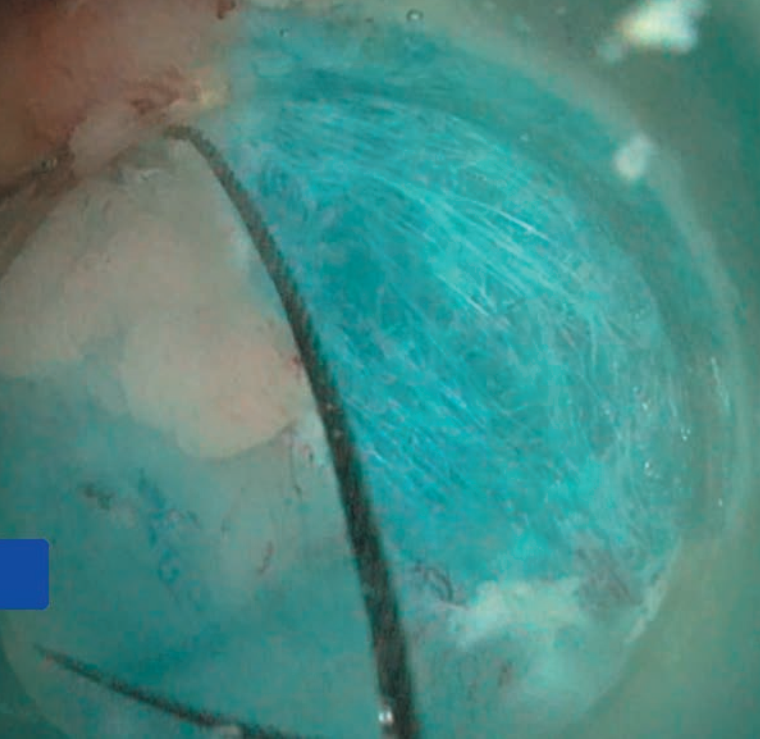
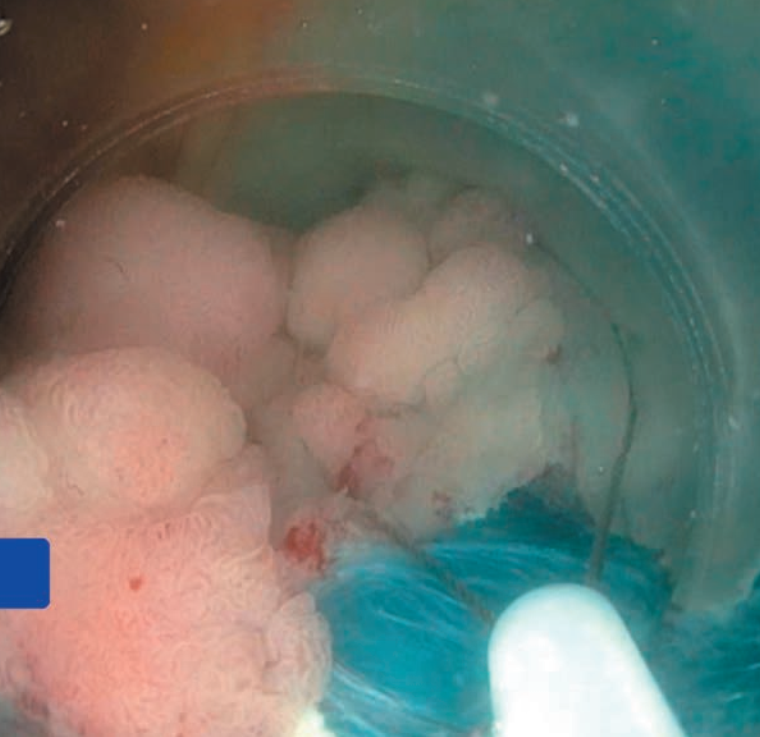
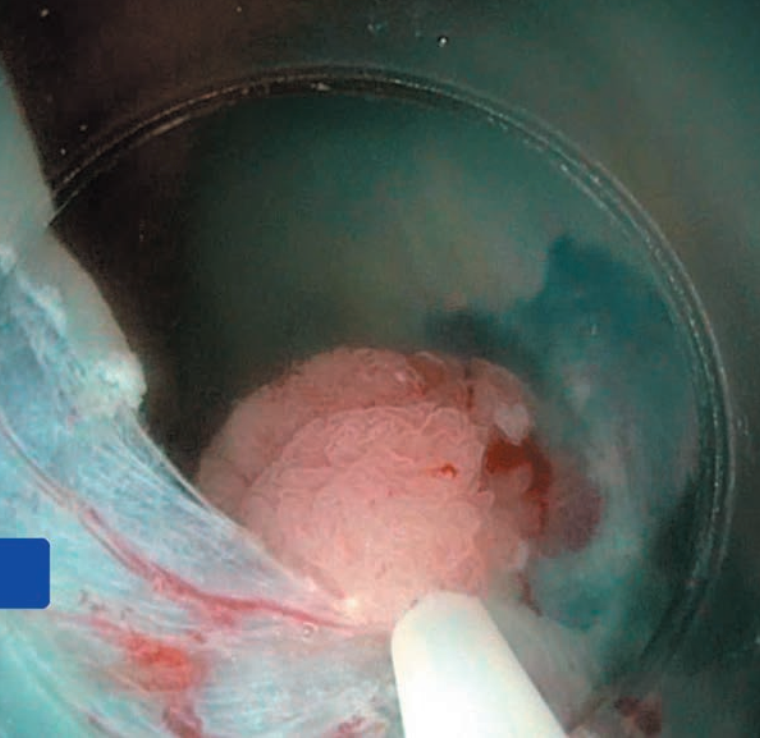
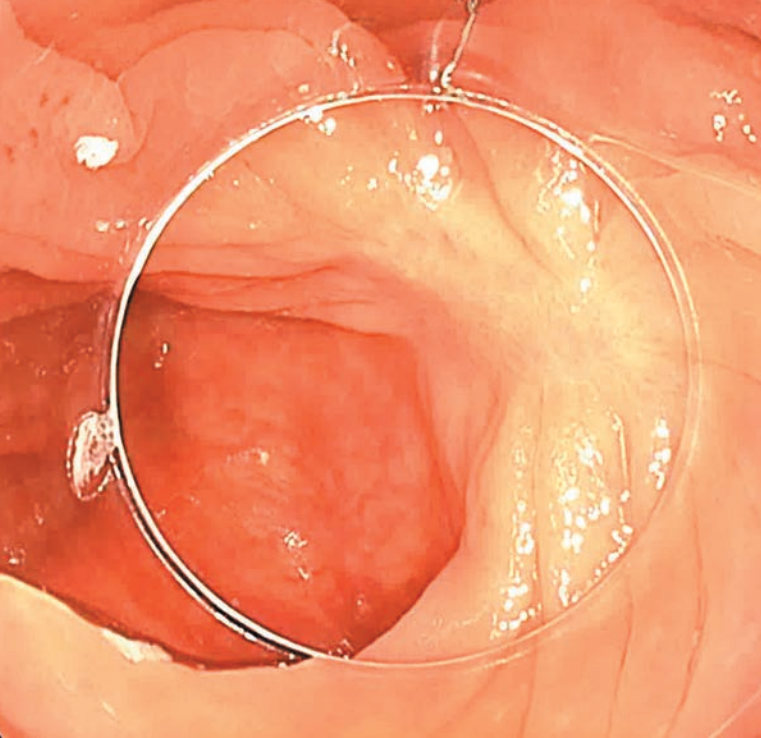
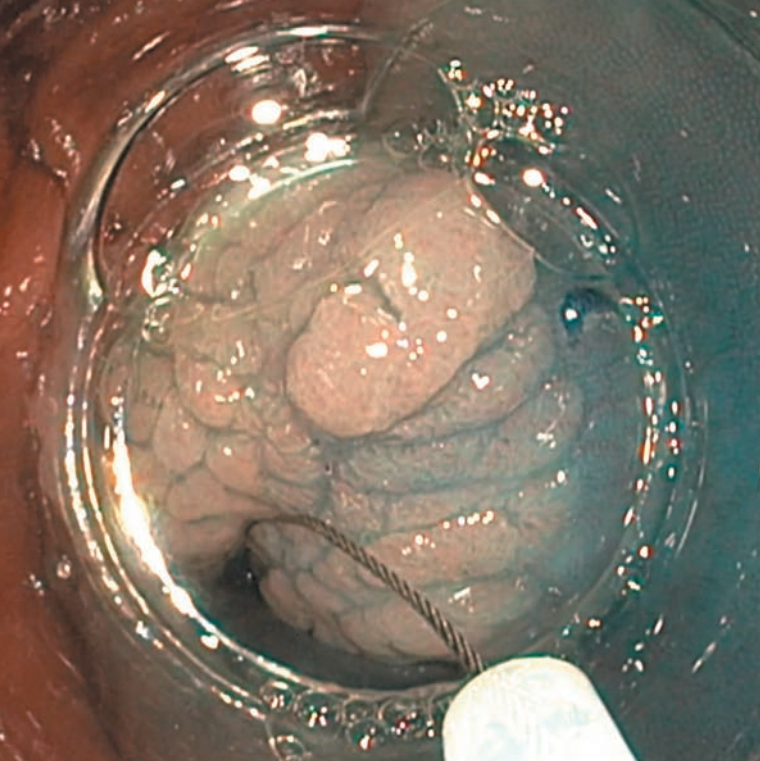
1I inject the dye solution into the submucosal layer in order to lift a specific fragment rather than the entire lesion (Fig. 3A, Fig. 3C, Fig. 2B). The created submucosal bubble is easily grasped with a snare (Fig. 4A, Fig. 5A, Fig. 4C, Fig. 5C). I prevent „smoothing” of the surface or „collapsing” of the edges of the lesion by injecting a large amount of solution under the entire lesion at once.
2When injecting the solution, I change the angle of the needle without changing the injection site. I avoid numerous injections. Often instead of the solution administered through the needle, I use water-jet to lift the lesion during the procedure, injecting water directly from the endoscope – this shortens the time of the procedure.
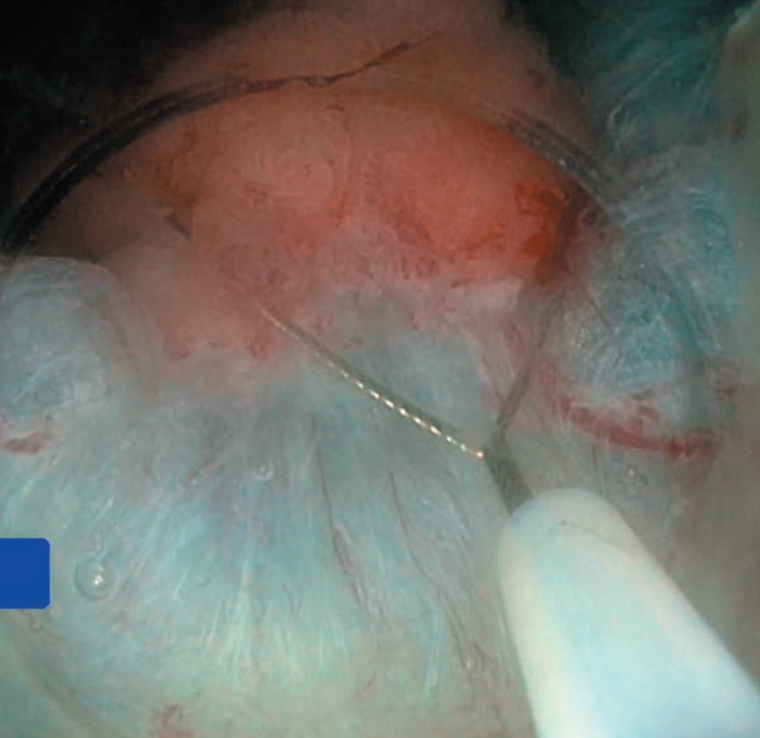
3I start the resection by removing the edges of the lesion with a margin of healthy mucosa. When removing the edges of the lesion I often remove relatively large areas of healthy mucosa bordering the lesion (Fig. 4A, Fig. 6C, Fig. 4B, Fig. 5B, Fig. 6B). The use of a thin braided snare facilitates the grasping of healthy tissue located around the lesion. At this stage, the use of electrocoagulation is often not necessary and can be kept to a minimum.
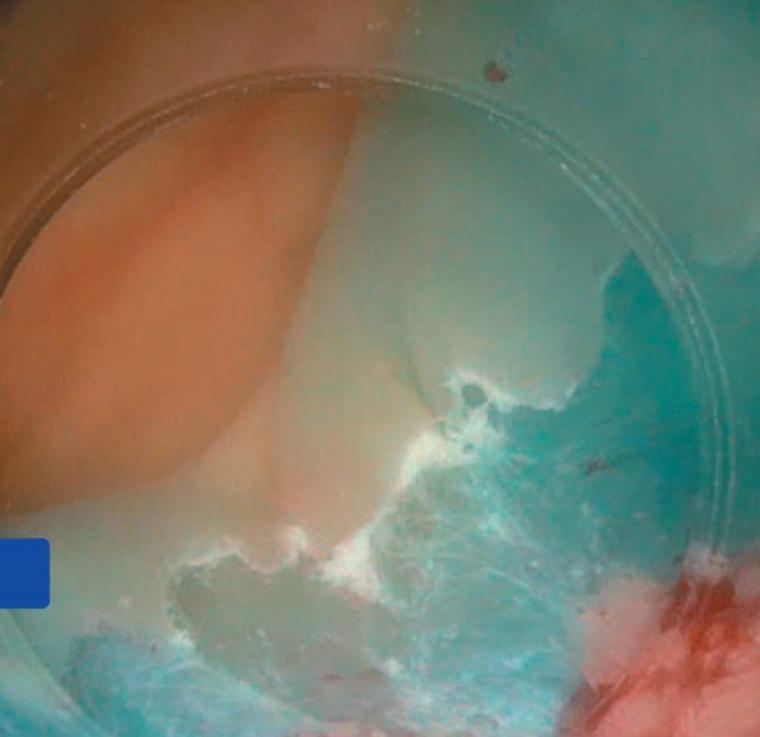
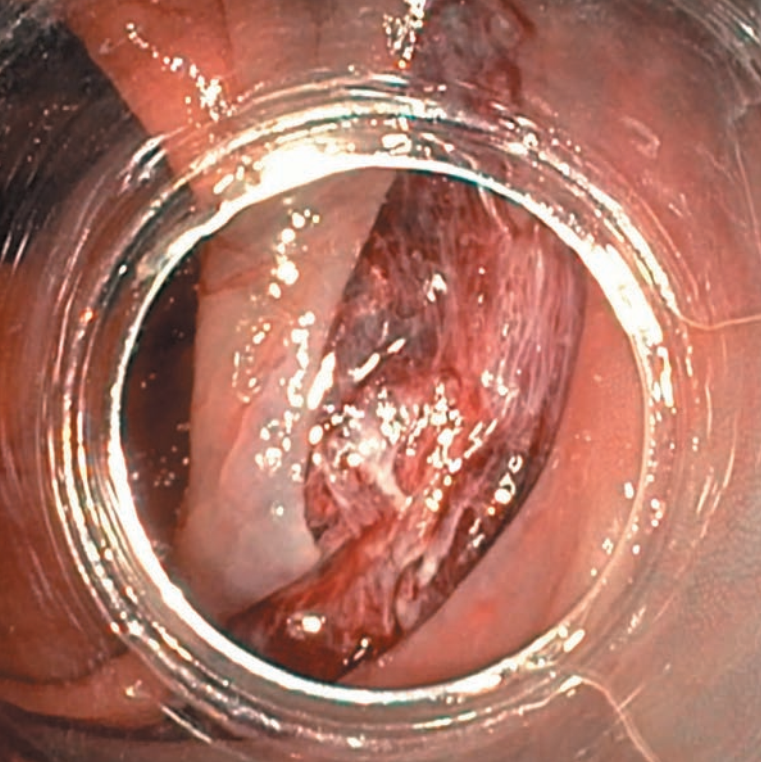
4Performing a complete circular resection of the edges of the lesion facilitates „mobilisation” and removal of the central part of the lesion. Fibrosis in the submucosal layer is usually most significant in this part of the lesion (Fig. 13B). Before removing the central part of the lesion, I make sure that the marginal resection is complete (Figs. 8A-10A).
5Fibrosis in the submucosal layer, may be the cause of the non-lifting sign. To remove non-lifting lesion fragments, I use a stiff, thin wire snare (Fig. 11A, Fig. 11B, Fig. 12B). Electrocoagulation is usually necessary to remove these fragments.
6Most serrated lesions and a large proportion of classical adenomas especially with 0-IIa, 0-IIb morphology, can be removed by cold EMR technique (Case C).
7 Filling the bowel with water facilitates capturing the edge of the lesion with a wide margin of healthy tissue (Fig. 6A, Fig. 7A, Fig. 4B, Fig. 5B, Fig. 6B), removing areas with non-lifting sign (Fig. 11A, Fig. 11B, Fig. 12B, Fig. 13B) and careful evaluation of the EMR site (Fig. 8A, Fig. 9A, Fig. 10A, Fig. 13A, Figs. 10C-12C, Fig. 3B, Figs. 7B-10B).
8The transparent distal cap facilitates the procedure in most cases, increasing stability and facilitating access to fragments of the lesion with difficult location.
Case A
EMR of a lesion type LST G-H (0-IIa), located in the ascending colon, size – 30 mm.





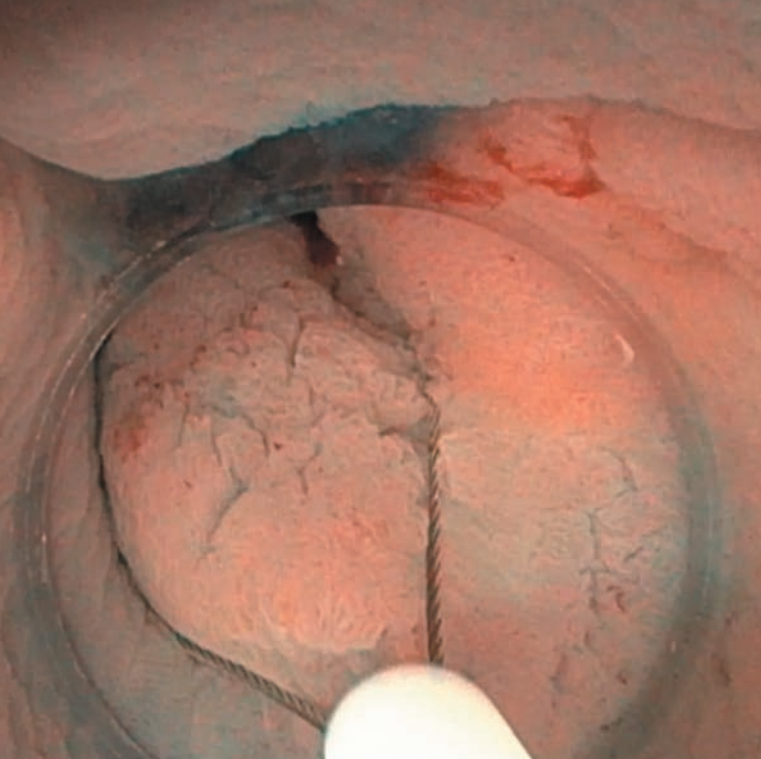







Case B
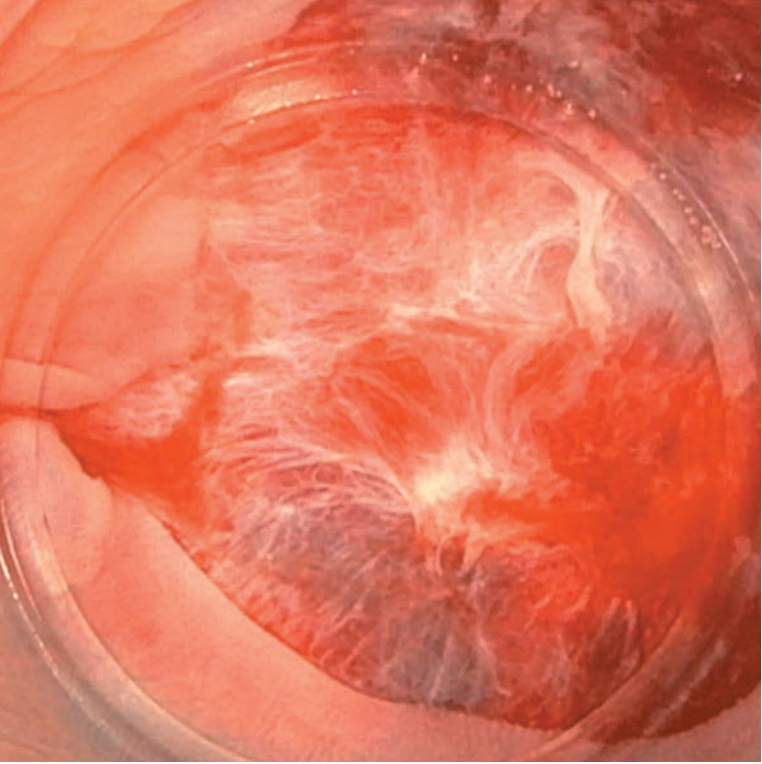
EMR of LST G-NM (0-Is) type lesion, located in the transverse colon, with intense fibrosis in the central part, size – 35 mm. The procedure performed mostly in water immersion (SnareMaster Plus 15 mm).


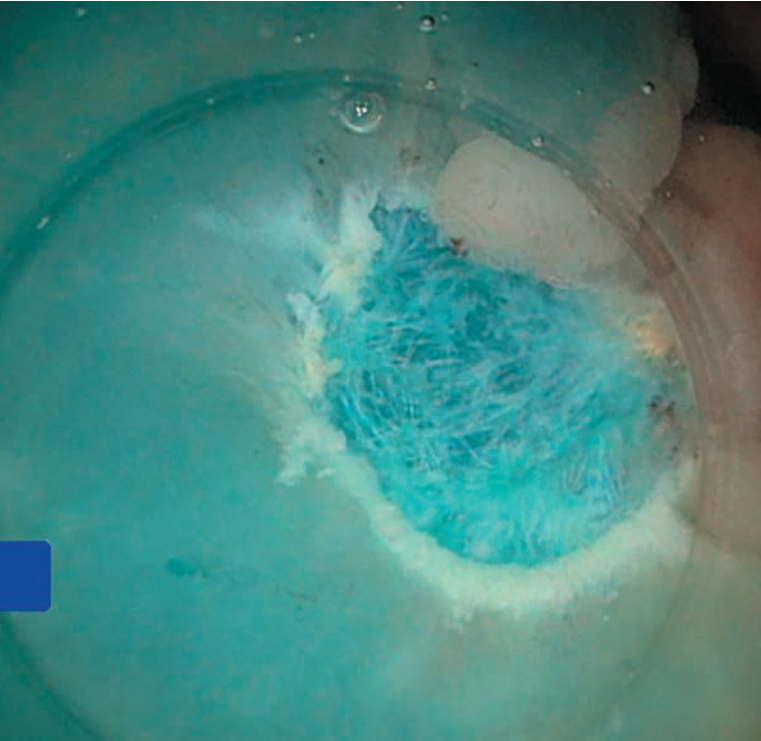





Case C
Cold EMR of the LST G-H (0-IIa) type of lesion, located in the ascending colon, size – 20 mm .









- Keyword
- Content Type